Happy Birthday, BTM! A Year in Expert Care, Discovery and Innovation
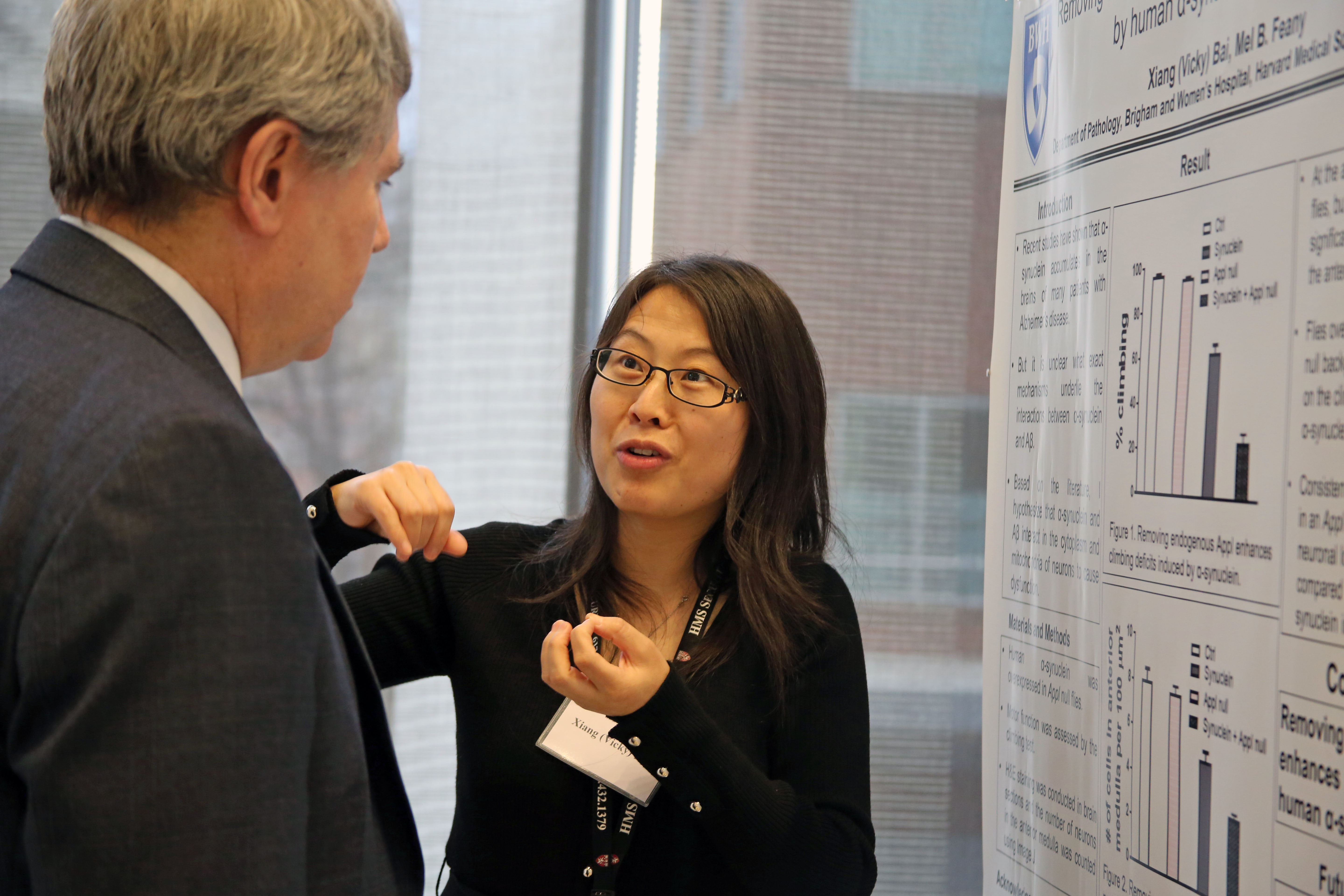
The Building for Transformative Medicine (BTM) opened its doors to patients last October as a hub for state-of-the-art labs, outpatient clinical space and advanced imaging facilities. Located at 60 Fenwood Road, the building brings together researchers and clinicians from across multiple disciplines with a shared vision for collaboration, acceleration and translation of laboratory discoveries into novel treatments for patients.
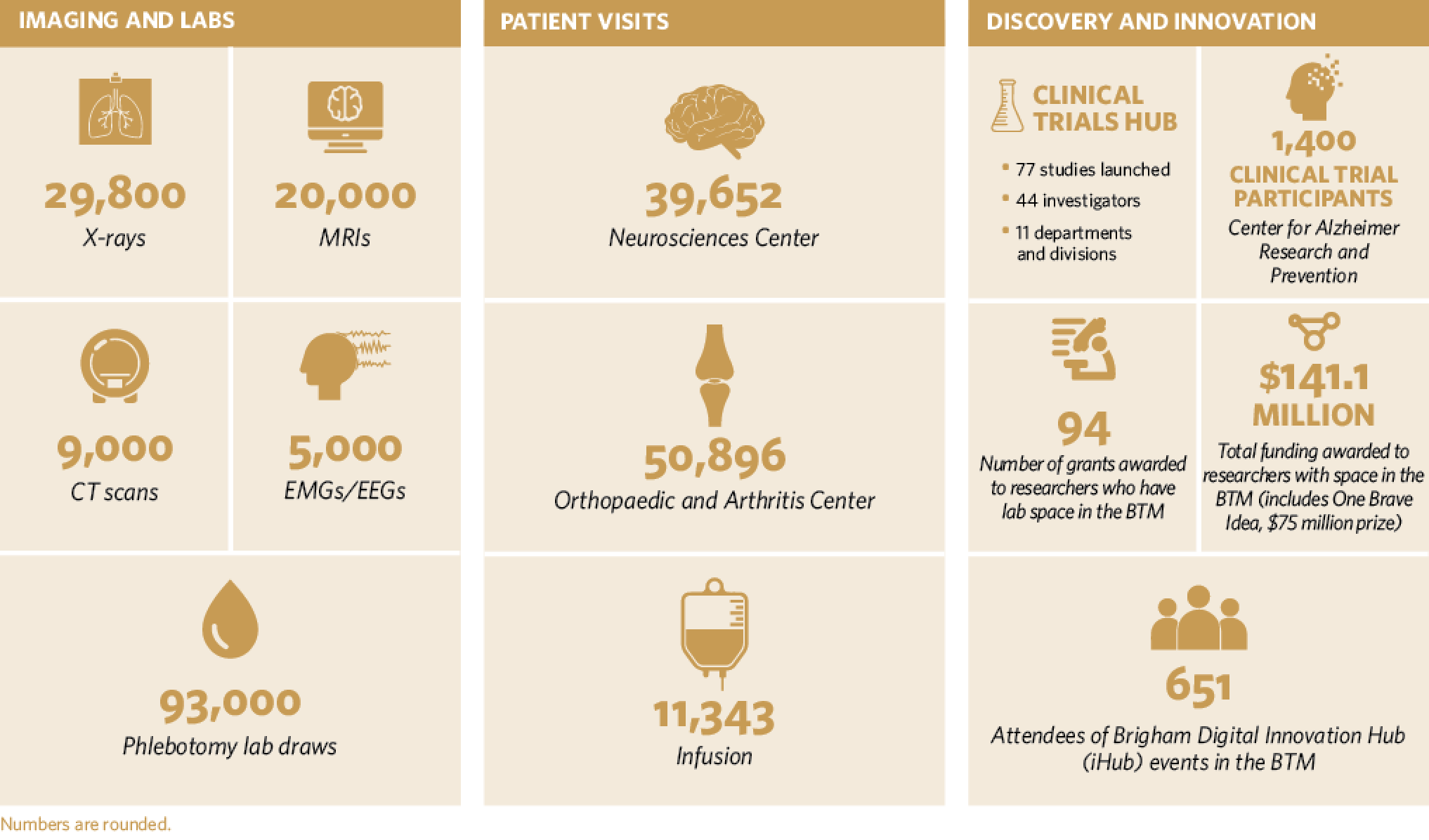
Here’s a look at the BTM’s first year, by the numbers, as of Sept. 30, 2017:



 O
O My proudest moment at BWH was receiving the Linda Morgante Hope Award: Best Work to Inspire Hope in MS at the Multiple Sclerosis Consortium with my colleagues in June 2016.
My proudest moment at BWH was receiving the Linda Morgante Hope Award: Best Work to Inspire Hope in MS at the Multiple Sclerosis Consortium with my colleagues in June 2016.






 The Weiner lab has an ambitious goal: to develop a nasal vaccine that will prevent and reverse the progression of Alzheimer’s disease.
The Weiner lab has an ambitious goal: to develop a nasal vaccine that will prevent and reverse the progression of Alzheimer’s disease.

 Anecdotal evidence of food allergies is everywhere, but exactly how common are these allergies and intolerances? In a new study, investigators from BWH analyzed data from medical records of more than 2.7 million patients across Partners HealthCare, identifying more than 97,000 with at least one documented food allergy or intolerance. Their findings were recently published in the Journal of Allergy and Clinical Immunology.
Anecdotal evidence of food allergies is everywhere, but exactly how common are these allergies and intolerances? In a new study, investigators from BWH analyzed data from medical records of more than 2.7 million patients across Partners HealthCare, identifying more than 97,000 with at least one documented food allergy or intolerance. Their findings were recently published in the Journal of Allergy and Clinical Immunology.

 Pointing to a recent cohort study and findings from randomized clinical trials, Manson said that there is an increasingly strong case for the link between the heart and brain. Traditional heart disease risk factors – smoking, hypertension, high cholesterol, diabetes and obesity – were found to correlate with the presence of amyloid plaques in the brain, a protein whose buildup is associated with Alzheimer’s.
Pointing to a recent cohort study and findings from randomized clinical trials, Manson said that there is an increasingly strong case for the link between the heart and brain. Traditional heart disease risk factors – smoking, hypertension, high cholesterol, diabetes and obesity – were found to correlate with the presence of amyloid plaques in the brain, a protein whose buildup is associated with Alzheimer’s.


 Investigators found that a single measurement of a novel biomarker for diabetes known as plasma glycated CD59 (GCD59), performed at weeks 24-28 of gestation, was able to identify women who had failed the standard of care screening test as well as women with confirmed gestational diabetes. The findings were published in a recent issue of Diabetes Care.
Investigators found that a single measurement of a novel biomarker for diabetes known as plasma glycated CD59 (GCD59), performed at weeks 24-28 of gestation, was able to identify women who had failed the standard of care screening test as well as women with confirmed gestational diabetes. The findings were published in a recent issue of Diabetes Care.






 The Brigham and Massachusetts General Hospital have teamed up to form the
The Brigham and Massachusetts General Hospital have teamed up to form the 










 A study led by BWH researchers in partnership with colleagues at Boston Children’s Hospital to explore the use of genome sequencing in newborns may give parents greater insight into their infants’ health.
A study led by BWH researchers in partnership with colleagues at Boston Children’s Hospital to explore the use of genome sequencing in newborns may give parents greater insight into their infants’ health.
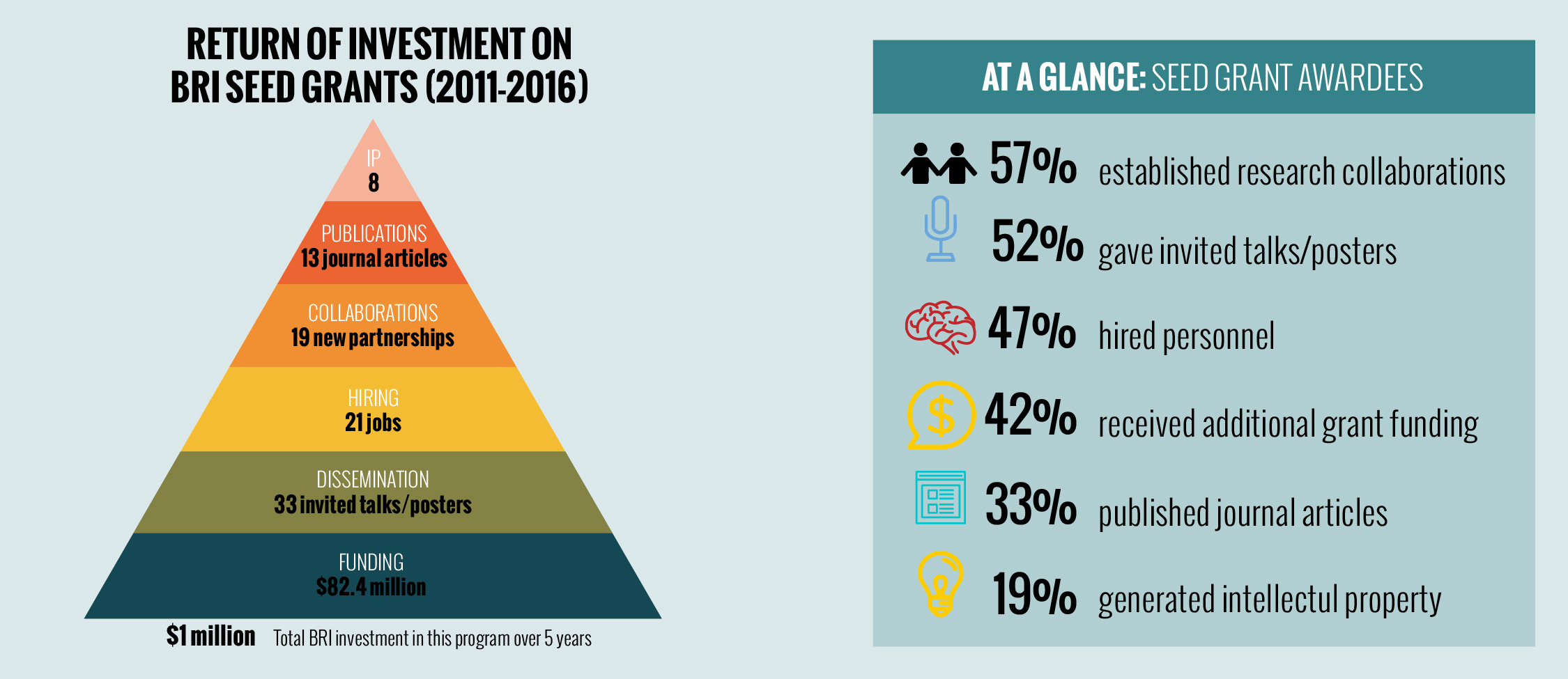 Early-stage funding from the Brigham Research Institute (BRI) has enabled 21 projects to flourish, according to recent feedback from award recipients.
Early-stage funding from the Brigham Research Institute (BRI) has enabled 21 projects to flourish, according to recent feedback from award recipients.














 21st Century Tools to Measure
21st Century Tools to Measure

 Detecting Early Neurological Decline
Detecting Early Neurological Decline