Joint Lab Will Pursue New Treatments for Chronic Lung Diseases

Senior leaders and scientists from Bayer, Brigham Health, Mass General and Partners HealthCare celebrate the new lab’s launch.
Scientists have studied lung diseases for decades, yet so much about them is still a mystery — including how they develop, why only certain people are afflicted with them and which treatments are most likely to be effective for any given patient.
Chronic lung disease is a broad term for several diseases of the airways and other structures of the lung, including chronic obstructive pulmonary disease (COPD). About 65 million people suffer from COPD and 3 million die from it each year, making it the third leading cause of death worldwide.
“The reality is that we don’t know what the key inciting events of COPD are, we don’t know how to reverse them therapeutically, and we’re not quite sure what the right molecular targets are,” explained Edwin Silverman, MD, PhD, chief of the Channing Division of Network Medicine. “We have a very rudimentary understanding of COPD. It’s an incomplete puzzle.”
 To help solve these unanswered questions and accelerate the search for lifesaving treatments, Brigham and Women’s Hospital, Massachusetts General Hospital and global pharmaceutical company Bayer announced the launch of a joint lab to research new drug candidates to treat chronic lung diseases. It will host scientists from all three parties, and Bayer is investing more than $30 million to fund joint research projects over the next five years.
To help solve these unanswered questions and accelerate the search for lifesaving treatments, Brigham and Women’s Hospital, Massachusetts General Hospital and global pharmaceutical company Bayer announced the launch of a joint lab to research new drug candidates to treat chronic lung diseases. It will host scientists from all three parties, and Bayer is investing more than $30 million to fund joint research projects over the next five years.
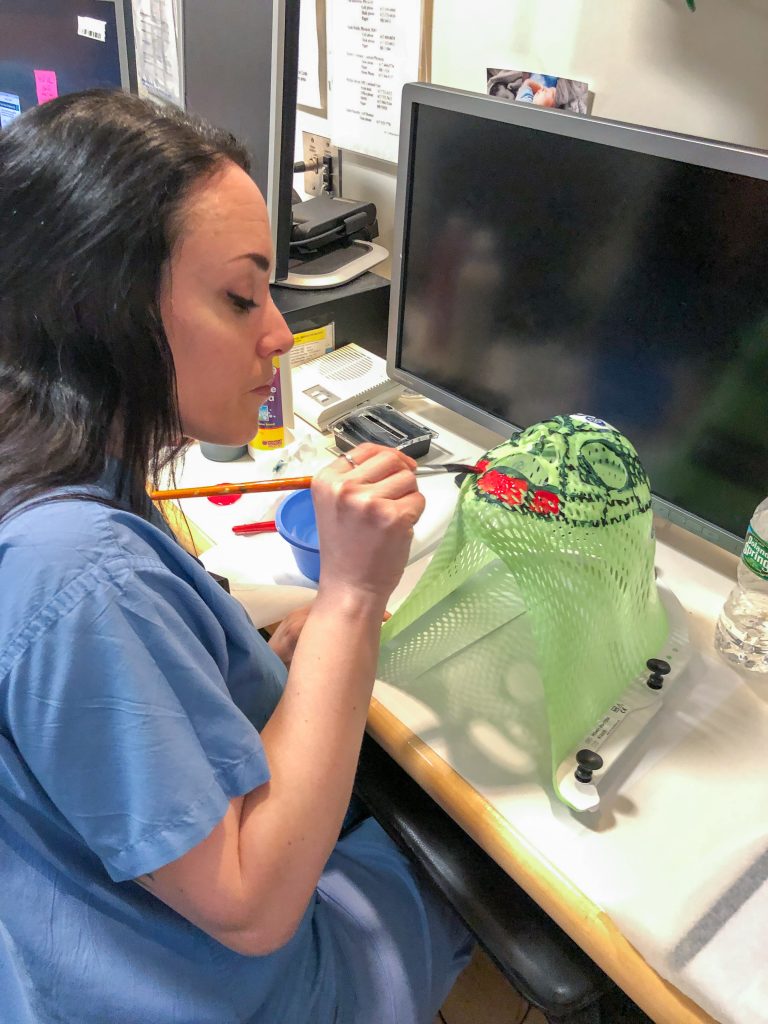
Scientists in the new joint lab will work side by side, combining Bayer’s capabilities in drug discovery and development with the complementary clinical expertise, understanding of disease mechanisms, data-analysis capabilities and insights from leading physician-scientists at the Brigham and Mass General. More than 20 people from the three organizations will work in combined teams in the lab, located in the Brigham’s Thorn Building. The rights to the research findings will be shared equally between the organizations.
“We strongly believe that this model will significantly accelerate the pace of discovery toward the goal of getting new therapies from the lab to patients safely and efficiently,” said Paul Anderson, MD, PhD, senior vice president and chief academic officer at the Brigham. “This collaboration provides the opportunity to integrate novel findings directly into the drug development pipeline, thus speeding up the time to move a new treatment into the clinic.”
Brigham Health President Betsy Nabel, MD, also underscored the importance of joint efforts like this, noting that academic medical centers can no longer rely solely on diminishing government grants for research funding.
“Programs like this are incredibly important to sustain our research mission,” Nabel said during an event celebrating the joint lab’s launch on Sept. 24.
Within the framework of the new collaboration, four leading experts will combine their expertise in the search for new treatment options for patients who suffer from chronic lung diseases. In addition to Silverman, the team consists of Bruce Levy, MD, chief of the Brigham’s Division of Pulmonary and Critical Care Medicine, Benjamin Medoff, MD, chief of Pulmonary and Critical Care at Mass General, and Markus Koch, PhD, head of Preclinical Research, Lung Diseases at Bayer.
“This collaboration is a terrific match of long-standing clinical and research excellence at Brigham Health and Mass General with Bayer’s drug development strength,” said Chris Coburn, chief innovation officer of Partners HealthCare. “This state-of-the-art partnership has emerged from a shared commitment to improving patients’ lives.”





 More than 400 patients have been referred to the Bridge Clinic since April 2018, and 75 percent of them came to at least one appointment. The average duration of care in the clinic is two and a half months. There is a cohort of patients that has remained with the Bridge Clinic for a longer period of up to 10 months, given their ongoing high acuity. Price said she’s thrilled with the progress that has been made in the clinic to help patients in need. In particular, the Bridge Clinic’s 83 percent retention rate — representing patients who continue to receive treatment at the clinic or in longitudinal care after six months — outshines national averages for similar programs, which rarely reach 50 percent.
More than 400 patients have been referred to the Bridge Clinic since April 2018, and 75 percent of them came to at least one appointment. The average duration of care in the clinic is two and a half months. There is a cohort of patients that has remained with the Bridge Clinic for a longer period of up to 10 months, given their ongoing high acuity. Price said she’s thrilled with the progress that has been made in the clinic to help patients in need. In particular, the Bridge Clinic’s 83 percent retention rate — representing patients who continue to receive treatment at the clinic or in longitudinal care after six months — outshines national averages for similar programs, which rarely reach 50 percent.












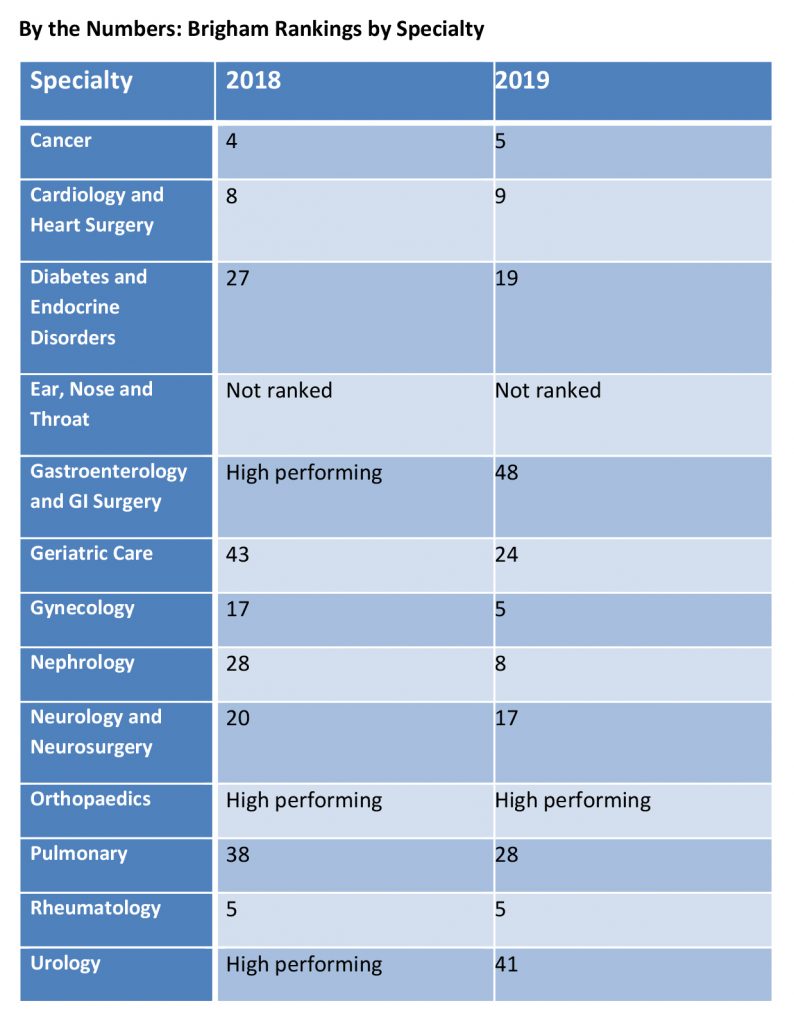
 Brigham and Women’s Hospital rose to No. 13 on the 2019 U.S. News & World Report’s ranking of Best Hospitals, up from No. 20 in last year’s annual Honor Roll. The Honor Roll is a distinction awarded to 20 hospitals that deliver exceptional treatment across multiple areas of care.
Brigham and Women’s Hospital rose to No. 13 on the 2019 U.S. News & World Report’s ranking of Best Hospitals, up from No. 20 in last year’s annual Honor Roll. The Honor Roll is a distinction awarded to 20 hospitals that deliver exceptional treatment across multiple areas of care.