Brigham Team Recognized for Role in Disaster Response
 When a major flood caused by a burst pipe forced the closure of the labor and delivery and neonatal intensive care units at Boston Medical Center (BMC) temporarily last year, the Brigham and several other hospitals stepped up to ensure patient care remained the priority.
When a major flood caused by a burst pipe forced the closure of the labor and delivery and neonatal intensive care units at Boston Medical Center (BMC) temporarily last year, the Brigham and several other hospitals stepped up to ensure patient care remained the priority.
During a Quality Rounds presentation in Bornstein Amphitheater last month, BMC clinicians spoke about the flood and reflected on the disaster response and lessons learned.
A critical piece to the emergency plan for BMC was the safe and timely transfer of patients out of the affected units to area hospitals, including the Brigham, for care. At the end of Quality Rounds, the Brigham was presented with an award from BMC in recognition of the assistance staff provided during the flood incident.
Karen Fiumara, PharmD, BCPS, executive director of Patient Safety at Brigham Health, said the Brigham teams that responded to this challenging situation were “nothing short of remarkable.”
“While continuing to safely care for their existing patients, they welcomed this group of BMC patients and their loved ones to the Brigham with open arms and provided them with exceptional care,” Fiumara said. “This was one of those amazing stories that makes you proud to be part of the Brigham community.”
Katherine Gregory, PhD, RN, associate chief nursing officer for the Mary Horrigan Connors Center for Women and Newborns, echoed Fiumara’s thoughts.
“The Brigham comes together in a crisis like no other, and we care—not only about our patients but also those across the city and region,” she said. “It was our privilege to care for the women and newborns who were affected by the BMC flood last year, and we stand ready to serve if called upon by our obstetric and newborn colleagues again in the future.”



 Last summer, faculty and staff were invited to share their impressions of the Brigham’s organizational culture through the Brigham Experience: Culture, Diversity & Inclusion Assessment survey, focus groups, interviews and more. The message was clear: Our foundation and our people are strong, and we have opportunity to do even better, together.
Last summer, faculty and staff were invited to share their impressions of the Brigham’s organizational culture through the Brigham Experience: Culture, Diversity & Inclusion Assessment survey, focus groups, interviews and more. The message was clear: Our foundation and our people are strong, and we have opportunity to do even better, together. Many of you have already heard about the four amazing Brigham patient care assistants (PCAs) who received the inaugural Neskey Educational Opportunity Fund Scholarships, which provide full-tuition support to University of Massachusetts (UMass) Boston for PCAs who aspire to have a career in nursing. David and Sharon Neskey established the fund to honor the extraordinary care they received from a PCA here. As it turns out, the day we announced those four recipients was just one piece of what would become my One Shining Moment this year.
Many of you have already heard about the four amazing Brigham patient care assistants (PCAs) who received the inaugural Neskey Educational Opportunity Fund Scholarships, which provide full-tuition support to University of Massachusetts (UMass) Boston for PCAs who aspire to have a career in nursing. David and Sharon Neskey established the fund to honor the extraordinary care they received from a PCA here. As it turns out, the day we announced those four recipients was just one piece of what would become my One Shining Moment this year.
 My One Shining Moment for 2018 represents the culmination of many shining moments for the Department of Nursing and our entire Brigham community. After a journey led by our clinical nurses that inspired pride about the exceptional care we provide, our patient outcomes and our interprofessional collaboration, we officially received the news that Brigham and Women’s Hospital achieved Magnet designation.
My One Shining Moment for 2018 represents the culmination of many shining moments for the Department of Nursing and our entire Brigham community. After a journey led by our clinical nurses that inspired pride about the exceptional care we provide, our patient outcomes and our interprofessional collaboration, we officially received the news that Brigham and Women’s Hospital achieved Magnet designation.


 By far, my shining moment this year was the day I reconnected with my primary nurse, Vivian Kelley, RN, after 39 years! Vivian helped save my life back in 1979, when I came to the Peter Bent Brigham Hospital for a bone marrow transplant. I had aplastic anemia (a rare and life-threatening blood disease) and spent two and a half months in an isolation room. Vivian was there at every turn—when I got my chemo and during the hundreds of hours that followed as I waited for my new immune system to mature. The photo in which I’m wearing a mask marks the day I went home. The other picture was taken when we reconnected this summer in Boston. Vivian moved to the West Coast a year after my transplant and continued practicing nursing until she retired. I credit Vivian’s intelligence, nursing skills and her calm, positive attitude for getting me through a terrifying time in my life. I’m so grateful we found each other again.
By far, my shining moment this year was the day I reconnected with my primary nurse, Vivian Kelley, RN, after 39 years! Vivian helped save my life back in 1979, when I came to the Peter Bent Brigham Hospital for a bone marrow transplant. I had aplastic anemia (a rare and life-threatening blood disease) and spent two and a half months in an isolation room. Vivian was there at every turn—when I got my chemo and during the hundreds of hours that followed as I waited for my new immune system to mature. The photo in which I’m wearing a mask marks the day I went home. The other picture was taken when we reconnected this summer in Boston. Vivian moved to the West Coast a year after my transplant and continued practicing nursing until she retired. I credit Vivian’s intelligence, nursing skills and her calm, positive attitude for getting me through a terrifying time in my life. I’m so grateful we found each other again. Every year, Brigham and Women’s Hospital and Brigham and Women’s Faulkner Hospital participate as a team in the Boston Heart Walk and fundraise to support cardiovascular research and education, advocate for health and save lives. This walk is important to me because a few of my family members have experienced coronary artery disease, stroke and valve disease. By supporting the walk, I am doing my part to help fund current research that will make a difference for my family members and friends.
Every year, Brigham and Women’s Hospital and Brigham and Women’s Faulkner Hospital participate as a team in the Boston Heart Walk and fundraise to support cardiovascular research and education, advocate for health and save lives. This walk is important to me because a few of my family members have experienced coronary artery disease, stroke and valve disease. By supporting the walk, I am doing my part to help fund current research that will make a difference for my family members and friends.




 “When I got that diagnosis, it hit me like a brick. I thought, wow, there’s something else going on,” she said. “Genetically speaking, there’s no explanation for it.”
“When I got that diagnosis, it hit me like a brick. I thought, wow, there’s something else going on,” she said. “Genetically speaking, there’s no explanation for it.”

 Researchers found the strongest associations were related to mood and self-harm. Those who slept less than six hours were more than three times as likely to consider or attempt suicide, and they were four times as likely to report an attempted suicide that resulted in treatment. Only 30 percent of the students in the study reported averaging more than eight hours of sleep on school nights.
Researchers found the strongest associations were related to mood and self-harm. Those who slept less than six hours were more than three times as likely to consider or attempt suicide, and they were four times as likely to report an attempted suicide that resulted in treatment. Only 30 percent of the students in the study reported averaging more than eight hours of sleep on school nights.












 “Our staff’s commitment to service excellence, professionalism and team spirit came through loud and clear to the surveyors,” said Milenko Tanasijevic, MD, MBA, vice chair for Clinical Pathology and Quality. “They go above and beyond for every specimen and demonstrate their dedication to our patients every single day, regardless of whether a survey is occurring.”
“Our staff’s commitment to service excellence, professionalism and team spirit came through loud and clear to the surveyors,” said Milenko Tanasijevic, MD, MBA, vice chair for Clinical Pathology and Quality. “They go above and beyond for every specimen and demonstrate their dedication to our patients every single day, regardless of whether a survey is occurring.”
 “Through the years, the people we employ and the people we care for have become increasingly diverse. As our Brigham community evolves, our environment and culture must also evolve so that everyone who comes through our doors feels a sense of inclusion and belonging,” said Brigham Health President Betsy Nabel, MD, in a message to all staff.
“Through the years, the people we employ and the people we care for have become increasingly diverse. As our Brigham community evolves, our environment and culture must also evolve so that everyone who comes through our doors feels a sense of inclusion and belonging,” said Brigham Health President Betsy Nabel, MD, in a message to all staff.









 Now a trauma researcher in the Center for Surgery and Public
Now a trauma researcher in the Center for Surgery and Public 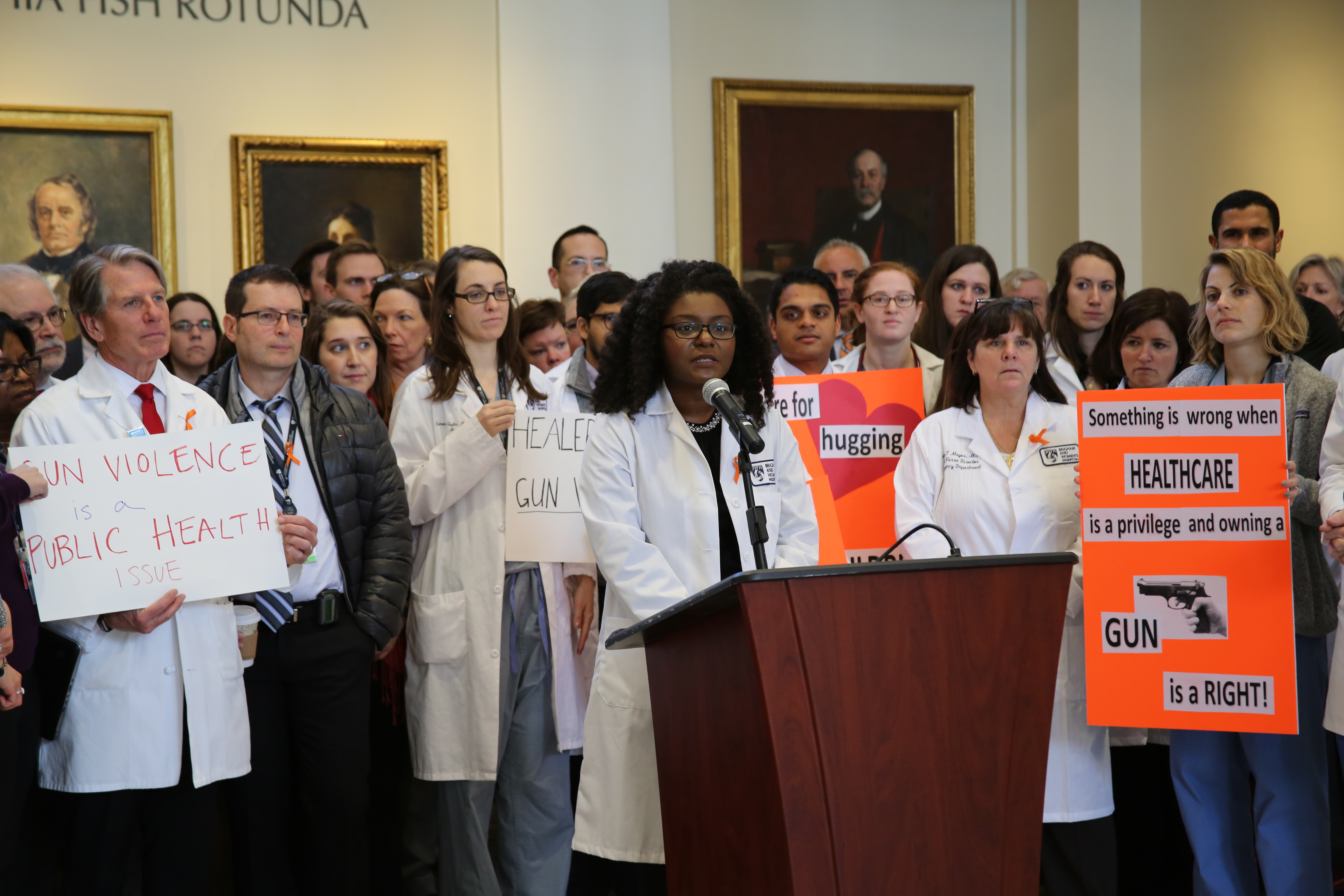
 At the Brigham, BWHers gathered in the Fish Rotunda at 15 Francis St. for a brief event, “Healers Stand Against Gun Violence,” hosted by the BWH Resident Social Justice Committee. Weeks and Charles Morris, MD, MPH, associate chief medical officer, offered reflections on gun violence as a public health issue. Chaplain Elizabeth (Elli) Goeke of Spiritual Care Services provided a moment of reflection in honor of all those affected by gun violence.
At the Brigham, BWHers gathered in the Fish Rotunda at 15 Francis St. for a brief event, “Healers Stand Against Gun Violence,” hosted by the BWH Resident Social Justice Committee. Weeks and Charles Morris, MD, MPH, associate chief medical officer, offered reflections on gun violence as a public health issue. Chaplain Elizabeth (Elli) Goeke of Spiritual Care Services provided a moment of reflection in honor of all those affected by gun violence.


 Another PIE Award recipient was Johann Brown, a dosimetrist (radiation planning expert) in the Department of Radiation Oncology. Brown was nominated for his tireless efforts to ensure patients receive timely care.
Another PIE Award recipient was Johann Brown, a dosimetrist (radiation planning expert) in the Department of Radiation Oncology. Brown was nominated for his tireless efforts to ensure patients receive timely care. One example of how these rounds led to improved care involved a patient with a serious brain injury who spent one year at the Brigham as an inpatient.
One example of how these rounds led to improved care involved a patient with a serious brain injury who spent one year at the Brigham as an inpatient.
 Massachusetts has been one of the states hit hardest by the nation’s opioid crisis, with the rate of opioid-related deaths seeing a fourfold increase between 2000 and 2015 across the state. In the span of just one year, 2013 to 2014, opioid-related deaths occurred in two-thirds of cities and towns in Massachusetts, according to the state Department of Public Health.
Massachusetts has been one of the states hit hardest by the nation’s opioid crisis, with the rate of opioid-related deaths seeing a fourfold increase between 2000 and 2015 across the state. In the span of just one year, 2013 to 2014, opioid-related deaths occurred in two-thirds of cities and towns in Massachusetts, according to the state Department of Public Health.
 “I didn’t think we were going to have enough hats, but then they poured in,” said Giller, who ultimately collected 550 hats, which are being distributed to infants in the Connors Center for Women and Newborns throughout February. “I am so grateful for every single hat that was made and for the people who helped spread the word. This would not be possible without everyone’s help.”
“I didn’t think we were going to have enough hats, but then they poured in,” said Giller, who ultimately collected 550 hats, which are being distributed to infants in the Connors Center for Women and Newborns throughout February. “I am so grateful for every single hat that was made and for the people who helped spread the word. This would not be possible without everyone’s help.”

 The message is still a poignant reminder of the duty health care institutions such as the Brigham have in propelling health equity and inclusion, Walls said.
The message is still a poignant reminder of the duty health care institutions such as the Brigham have in propelling health equity and inclusion, Walls said.
 When the ED is at capacity, some patients leave after being seen by a triage nurse, but before being seen by a physician. When a “walkout” occurs – often due to long wait times – it not only leads to a poor patient experience, but it is also a safety concern, as nearly 30 percent of patients who receive care in the Brigham’s ED are sick enough to be admitted.
When the ED is at capacity, some patients leave after being seen by a triage nurse, but before being seen by a physician. When a “walkout” occurs – often due to long wait times – it not only leads to a poor patient experience, but it is also a safety concern, as nearly 30 percent of patients who receive care in the Brigham’s ED are sick enough to be admitted.

 Mohamed El-Dib, MD, director of Neonatal Critical Care in the Department of Pediatric Newborn Medicine, is the principal investigator at BWH for a multi-institutional clinical trial looking at whether infusing babies with their own umbilical cord blood can indeed reverse tissue damage in the brain.
Mohamed El-Dib, MD, director of Neonatal Critical Care in the Department of Pediatric Newborn Medicine, is the principal investigator at BWH for a multi-institutional clinical trial looking at whether infusing babies with their own umbilical cord blood can indeed reverse tissue damage in the brain.
 Seltzer expressed his appreciation during a ceremony celebrating the unveiling of his portrait in Bornstein Amphitheater on Nov. 17. The portrait honors his contributions in medicine, science and education as the fourth chair of the Department of Radiology, a position he held from 1997 to 2016.
Seltzer expressed his appreciation during a ceremony celebrating the unveiling of his portrait in Bornstein Amphitheater on Nov. 17. The portrait honors his contributions in medicine, science and education as the fourth chair of the Department of Radiology, a position he held from 1997 to 2016.
 NICU staff also attended multidisciplinary workshops last fall hosted by the team, which incorporated training videos for staff that depicted various clinical scenarios, including how to properly perform hand hygiene and sterile tubing line changes. They also demonstrated collegial ways to approach someone who had not performed hand hygiene and was attempting to touch a patient.
NICU staff also attended multidisciplinary workshops last fall hosted by the team, which incorporated training videos for staff that depicted various clinical scenarios, including how to properly perform hand hygiene and sterile tubing line changes. They also demonstrated collegial ways to approach someone who had not performed hand hygiene and was attempting to touch a patient.
 “A patient may come to the Neurosurgery clinic for an appointment, and, after reviewing a case, we realize having one of our ENT specialists join us would be ideal,” Dunn said. “That can happen in real time rather than after scheduling a visit in another two weeks. It can be difficult for patients to return for multiple appointments, so we’re trying to deliver everything on site at once.”
“A patient may come to the Neurosurgery clinic for an appointment, and, after reviewing a case, we realize having one of our ENT specialists join us would be ideal,” Dunn said. “That can happen in real time rather than after scheduling a visit in another two weeks. It can be difficult for patients to return for multiple appointments, so we’re trying to deliver everything on site at once.”