BWHers Get Ready to Rock at Hurricane Relief Benefit Concert
The Big 6, a Harvard-based cover band formed by emergency physicians from the Brigham and staff from the Harvard Humanitarian Initiative (HHI), will hold a benefit concert on Sunday, Nov. 12, in Cambridge to raise funds for communities affected by hurricanes Harvey, Irma and Maria.
“We wanted to get help directly to the field,” said bass guitarist Valerie Dobiesz, MD, MPH, of the Department of Emergency Medicine. “We know monetary donations are the most effective way to make a difference at the local level, and a benefit concert seemed like a fun way to get people together in support of an important cause.”
 All proceeds from the event, hosted at Club Oberon, go directly to organizations providing humanitarian relief for affected areas, said singer and guitarist Michael VanRooyen, MD, MPH, chair of Emergency Medicine and founding director of HHI. The band will cover all expenses related to the performance and will match funds raised by ticket sales. In addition, a group of anonymous donors will provide matching funds.
All proceeds from the event, hosted at Club Oberon, go directly to organizations providing humanitarian relief for affected areas, said singer and guitarist Michael VanRooyen, MD, MPH, chair of Emergency Medicine and founding director of HHI. The band will cover all expenses related to the performance and will match funds raised by ticket sales. In addition, a group of anonymous donors will provide matching funds.
The concert will feature covers of classic and contemporary rock music.
Band members all regularly participate in domestic and international humanitarian efforts. They recently learned from organizations they often work with that donations toward relief efforts had dropped off as this year’s devastating hurricane season went on.
“Contributions came in quickly for Texas with Harvey, then less funding came in for Irma for Florida. By the time Maria hit Puerto Rico, there was much less support because of donor fatigue,” VanRooyen said.
Playing an active role in providing relief efforts all around the world is part of the Brigham’s culture, VanRooyen said. A benefit concert offers a great opportunity to encourage more people to contribute to relief efforts, he added.
“People who are affected by crises like these are their own best resource,” VanRooyen said. “They do the hard work. All we’re doing is lending a helping hand.”
Since forming last fall, The Big 6 has played mostly in smaller, private settings. Although this performance marks the band’s first concert in a larger venue, its members are excited to take the leap.
“There’s no pressure at all. We take it seriously because we try to do well, but we just have a hilarious amount of fun together, and I think that translates every time we perform,” VanRooyen said. “If we can get a bunch of our friends and colleagues together and have fun for a good cause, then that is worth the price of admission.”
Rhythm guitarist and vocalist Tim Erickson, MD, chief of Emergency Medicine’s Division of Medical Toxicology, agreed that The Big Six – including its other members from HHI, Sam Plasmati and Isaac Baker – is excited for the big night.
“We love playing together, but it’s important for us that it’s for a cause and has an impact,” Erickson said. “We feel really blessed to have an opportunity to help.”
The Big Six Hurricane Relief Concert is Sunday, Nov. 12, 7 p.m., at Club Oberon, 2 Arrow St., Cambridge. To purchase tickets, click here or call 617-495-2668.


 You’re also a preceptor. What do you enjoy about educating PA students?
You’re also a preceptor. What do you enjoy about educating PA students?
 “Bullying is symptomatic of a larger issue around inclusion and respect,” said Sabrina Williams, MBA, chief diversity and inclusion officer and interim vice president of Human Resources, who served as moderator for the Oct. 2 event.
“Bullying is symptomatic of a larger issue around inclusion and respect,” said Sabrina Williams, MBA, chief diversity and inclusion officer and interim vice president of Human Resources, who served as moderator for the Oct. 2 event.
 While this was not Tracy’s first endurance event, it was by far her longest. Several years ago, she competed in an Ironman Triathlon – consisting of a 2.4-mile swim, a 112-mile bike ride and a 26.2-mile marathon. Prior to that, she competed in 100-mile rides and even one 120-mile race.
While this was not Tracy’s first endurance event, it was by far her longest. Several years ago, she competed in an Ironman Triathlon – consisting of a 2.4-mile swim, a 112-mile bike ride and a 26.2-mile marathon. Prior to that, she competed in 100-mile rides and even one 120-mile race.
 The website provides easy access to an extensive array of BWH departments and services, including Information Services (IS), Security, environmental chemical waste collection, Interpreter Services, Audiovisual Services and more.
The website provides easy access to an extensive array of BWH departments and services, including Information Services (IS), Security, environmental chemical waste collection, Interpreter Services, Audiovisual Services and more.
 BARMC reached out to the MHA to seek support as the facility and its staff recover from the hurricane. Many staff members have lost their homes to the floodwaters, and they have been fighting exhaustion to stay on the job and deal with a spike in emergency department visits.
BARMC reached out to the MHA to seek support as the facility and its staff recover from the hurricane. Many staff members have lost their homes to the floodwaters, and they have been fighting exhaustion to stay on the job and deal with a spike in emergency department visits. Knowing she wasn’t in the position to travel and help in person, Hardiman, a mother of four and a nurse in the ICU Float Pool, said she wanted to do something else to contribute to hurricane relief efforts. She solicited donations from family and friends via Facebook. Within minutes, people responded saying they also wanted to donate.
Knowing she wasn’t in the position to travel and help in person, Hardiman, a mother of four and a nurse in the ICU Float Pool, said she wanted to do something else to contribute to hurricane relief efforts. She solicited donations from family and friends via Facebook. Within minutes, people responded saying they also wanted to donate.
 During his treatment, however, other aspects of Thurber’s health began to deteriorate. He couldn’t walk. He needed supplemental oxygen to breathe. Baffled by this sharp decline, Thurber’s physicians recommended he go to Boston to see specialists at BWH.
During his treatment, however, other aspects of Thurber’s health began to deteriorate. He couldn’t walk. He needed supplemental oxygen to breathe. Baffled by this sharp decline, Thurber’s physicians recommended he go to Boston to see specialists at BWH.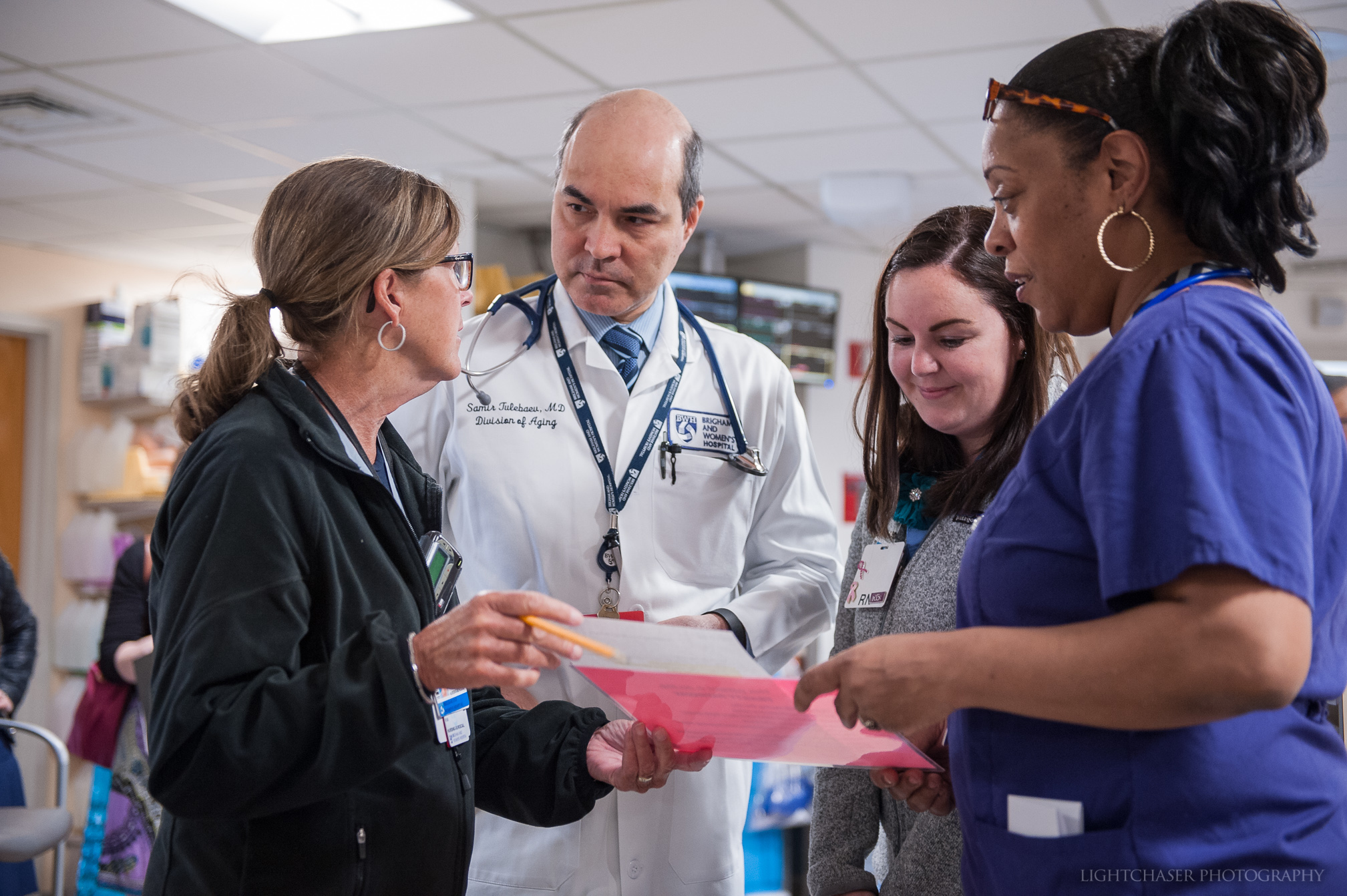
 As part of this journey, staff are invited to contribute to an interactive display in the 75 Francis St. lobby by sharing how they exemplify four hallmarks of Magnet institutions – high-quality patient care, clinical excellence, innovations in professional practice and interprofessional collaboration – in their daily work. Stickers provided at a nearby table encourage staff to write about how their role exemplifies one or more of those categories.
As part of this journey, staff are invited to contribute to an interactive display in the 75 Francis St. lobby by sharing how they exemplify four hallmarks of Magnet institutions – high-quality patient care, clinical excellence, innovations in professional practice and interprofessional collaboration – in their daily work. Stickers provided at a nearby table encourage staff to write about how their role exemplifies one or more of those categories.
 Williams has more than 15 years of experience as an HR senior executive. Prior to joining the Brigham, she was vice president of Human Resources at Neighborhood Health Plan. Prior to her role at NHP, she served as director of Human Resources for the Health Science Campuses at Tufts University. She has also held leadership roles at several nonprofit organizations, including the Urban League of Eastern Massachusetts, South End Settlements and the Roxbury Community College Foundation.
Williams has more than 15 years of experience as an HR senior executive. Prior to joining the Brigham, she was vice president of Human Resources at Neighborhood Health Plan. Prior to her role at NHP, she served as director of Human Resources for the Health Science Campuses at Tufts University. She has also held leadership roles at several nonprofit organizations, including the Urban League of Eastern Massachusetts, South End Settlements and the Roxbury Community College Foundation. The Weiner lab has an ambitious goal: to develop a nasal vaccine that will prevent and reverse the progression of Alzheimer’s disease.
The Weiner lab has an ambitious goal: to develop a nasal vaccine that will prevent and reverse the progression of Alzheimer’s disease.

 Corbin and Erin McDonough, MBA, senior vice president and chief communication officer, held 16 half-hour sessions in Bornstein Amphitheater over two days. During the event, employees viewed the videos, learned tactics to prevent tailgating and engaged in discussion.
Corbin and Erin McDonough, MBA, senior vice president and chief communication officer, held 16 half-hour sessions in Bornstein Amphitheater over two days. During the event, employees viewed the videos, learned tactics to prevent tailgating and engaged in discussion.

 That nurse was John Solman, RN, who was one of eight Brigham nurses honored during the 17th annual Internal Medicine Nursing Awards on June 8. Residents established the awards to recognize nurses for their commitment to care and mentorship.
That nurse was John Solman, RN, who was one of eight Brigham nurses honored during the 17th annual Internal Medicine Nursing Awards on June 8. Residents established the awards to recognize nurses for their commitment to care and mentorship.
 Pharmacy students on the team have a lot of face-to-face conversations with patients about medication management. Students counsel patients about their medications and assess barriers to medication adherence.
Pharmacy students on the team have a lot of face-to-face conversations with patients about medication management. Students counsel patients about their medications and assess barriers to medication adherence. In April, BWH submitted evidence of the hospital’s commitment to quality patient care, clinical excellence, interprofessional collaboration and innovation for consideration as a Magnet-designated hospital. While the Magnet Recognition Program’s roots are in nursing, the designation honors the work and culture of an entire institution.
In April, BWH submitted evidence of the hospital’s commitment to quality patient care, clinical excellence, interprofessional collaboration and innovation for consideration as a Magnet-designated hospital. While the Magnet Recognition Program’s roots are in nursing, the designation honors the work and culture of an entire institution.
 Pointing to a recent cohort study and findings from randomized clinical trials, Manson said that there is an increasingly strong case for the link between the heart and brain. Traditional heart disease risk factors – smoking, hypertension, high cholesterol, diabetes and obesity – were found to correlate with the presence of amyloid plaques in the brain, a protein whose buildup is associated with Alzheimer’s.
Pointing to a recent cohort study and findings from randomized clinical trials, Manson said that there is an increasingly strong case for the link between the heart and brain. Traditional heart disease risk factors – smoking, hypertension, high cholesterol, diabetes and obesity – were found to correlate with the presence of amyloid plaques in the brain, a protein whose buildup is associated with Alzheimer’s.
 “Daphne is a brilliant physician-scientist who cares deeply about her patients,” Nabel said. “She’s also a very thoughtful and collaborative leader who brings a depth of experience, not only in patient care, research innovation and teaching, but also administratively. The chemistry was a perfect fit.”
“Daphne is a brilliant physician-scientist who cares deeply about her patients,” Nabel said. “She’s also a very thoughtful and collaborative leader who brings a depth of experience, not only in patient care, research innovation and teaching, but also administratively. The chemistry was a perfect fit.”
 Investigators found that a single measurement of a novel biomarker for diabetes known as plasma glycated CD59 (GCD59), performed at weeks 24-28 of gestation, was able to identify women who had failed the standard of care screening test as well as women with confirmed gestational diabetes. The findings were published in a recent issue of Diabetes Care.
Investigators found that a single measurement of a novel biomarker for diabetes known as plasma glycated CD59 (GCD59), performed at weeks 24-28 of gestation, was able to identify women who had failed the standard of care screening test as well as women with confirmed gestational diabetes. The findings were published in a recent issue of Diabetes Care.
 Three BWHers received the
Three BWHers received the