A Tribute to the Legacy of the Rev. Dr. Martin Luther King Jr.

The Brigham chapter of the Association for Multicultural Members of Partners (AMMP) invites you to attend its annual celebration of the life and legacy of the Rev. Dr. Martin Luther King Jr.
Join AMMP on Tuesday, Jan. 22, noon-1 p.m., in Bornstein Amphitheater, for a panel discussion on the “Impact of Serving Others.” The panel will discuss service in the context of empowering individuals, strengthening communities and developing solutions to many of today’s social and economic challenges.
The panel will include individuals who have dedicated decades of their lives to service: Michael Curry, immediate past president, Boston Chapter of the National Association for the Advancement of Colored People (NAACP), board member, NAACP and senior vice president and general counsel at the Massachusetts League of Community Health Centers; Kim Janey, Boston city councilor, District 7; Nia Evans, co-founder and director, Boston Ujima Project; and Shelita Bailey, director, Workforce Development and Volunteer Services, Brigham and Women’s Hospital.
All are welcome to attend. Lunch will be provided. This event will also be webcast.






 There were so many shining moments throughout 2018, but what brings me the most joy this holiday season are the decorative birch trees displayed across our main campus. These trees celebrate our partnerships with dozens of organizations that support our friends and neighbors in our local community, providing vital services to improve their quality of life.
There were so many shining moments throughout 2018, but what brings me the most joy this holiday season are the decorative birch trees displayed across our main campus. These trees celebrate our partnerships with dozens of organizations that support our friends and neighbors in our local community, providing vital services to improve their quality of life.
 Every year, Brigham and Women’s Hospital and Brigham and Women’s Faulkner Hospital participate as a team in the Boston Heart Walk and fundraise to support cardiovascular research and education, advocate for health and save lives. This walk is important to me because a few of my family members have experienced coronary artery disease, stroke and valve disease. By supporting the walk, I am doing my part to help fund current research that will make a difference for my family members and friends.
Every year, Brigham and Women’s Hospital and Brigham and Women’s Faulkner Hospital participate as a team in the Boston Heart Walk and fundraise to support cardiovascular research and education, advocate for health and save lives. This walk is important to me because a few of my family members have experienced coronary artery disease, stroke and valve disease. By supporting the walk, I am doing my part to help fund current research that will make a difference for my family members and friends.










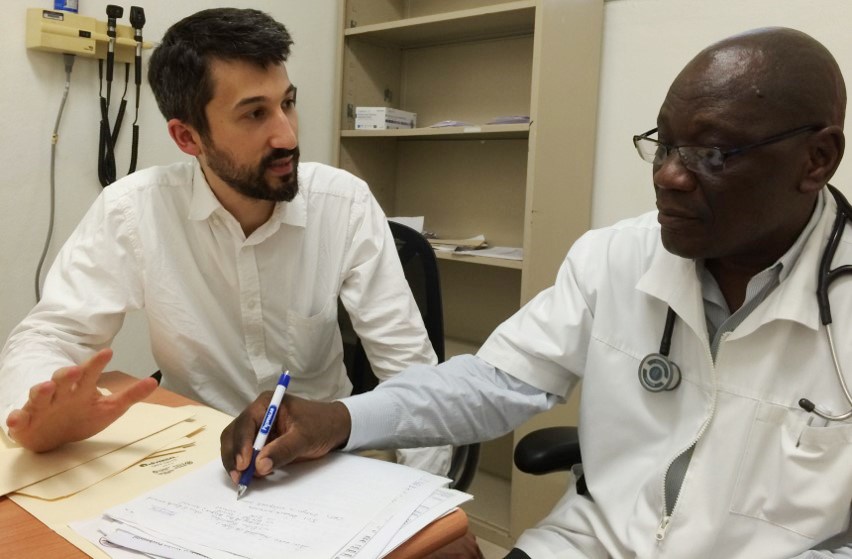

 Ongoing since September 2017, the “Wednesday Wellness” series takes place twice a month at the Brigham and Women’s Center for Community Wellness, Dorchester, located within Sportsmen’s. Each course focuses on a different health- and wellness-related topic, with more than 20 sessions held to date. Courses have covered diabetes and hypertension, dementia and arthritis, among other topics.
Ongoing since September 2017, the “Wednesday Wellness” series takes place twice a month at the Brigham and Women’s Center for Community Wellness, Dorchester, located within Sportsmen’s. Each course focuses on a different health- and wellness-related topic, with more than 20 sessions held to date. Courses have covered diabetes and hypertension, dementia and arthritis, among other topics.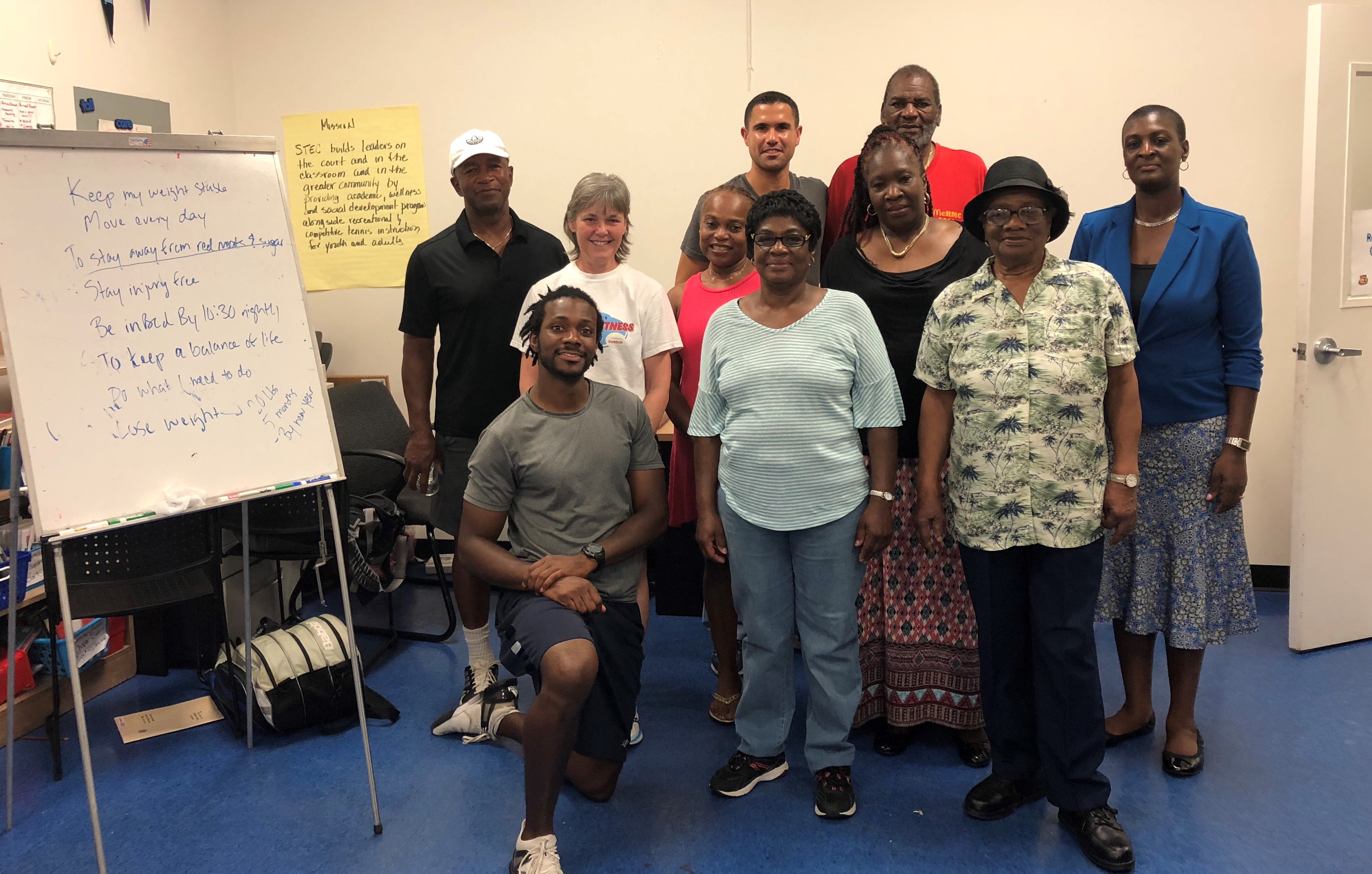






 Donations fill a red sleigh in the lobby at 75 Francis St. By the end of this year’s drive, it overflowed with a variety of colorful toys, including board games, soccer balls and dolls. One hundred Beanie Babies – donated by Ron M. Walls, MD, Brigham Health executive vice president and chief operating officer – lined nearly every surface.
Donations fill a red sleigh in the lobby at 75 Francis St. By the end of this year’s drive, it overflowed with a variety of colorful toys, including board games, soccer balls and dolls. One hundred Beanie Babies – donated by Ron M. Walls, MD, Brigham Health executive vice president and chief operating officer – lined nearly every surface.














 T
T





