NICU OT Ensures the Brigham’s Littlest Patients Are Prepared for Long-Term Success

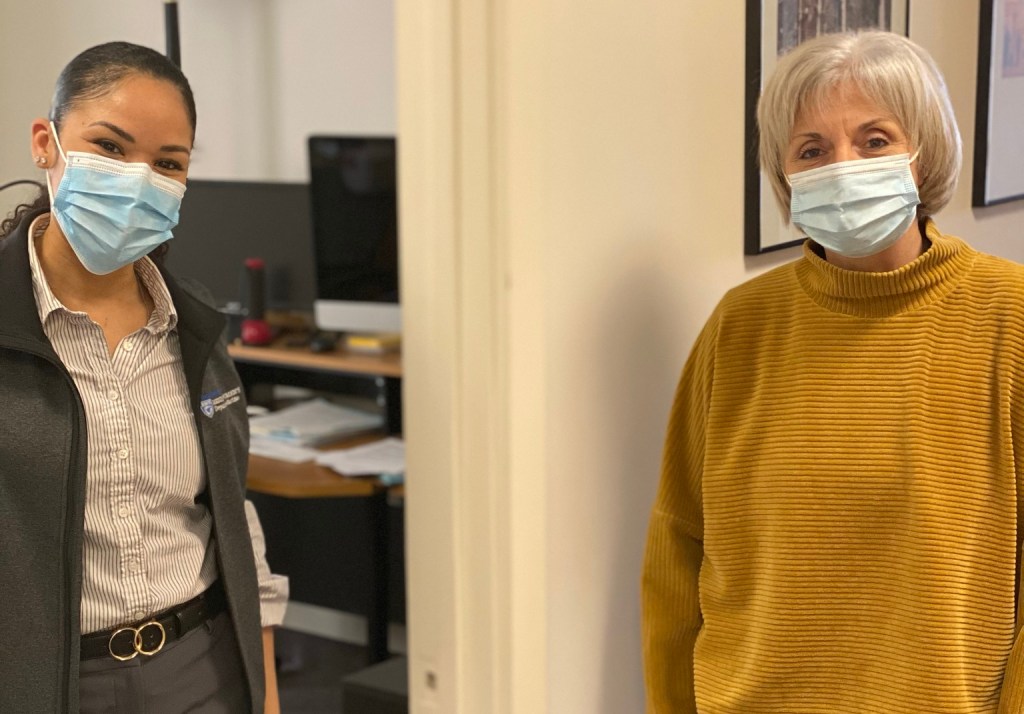
Jessica Pacheco is the only occupational therapist for the Brigham’s Neonatal Intensive Care Unit.
The goal of occupational therapy is to help people achieve independence for whatever it is that “occupies” their day. Jessica Pacheco, MOT, OTR/L, CNT, an occupational therapy clinical specialist in the Neonatal Intensive Care Unit (NICU) and NICU Follow-Up Program, is specially trained to help premature and medically complex babies participate in their “occupations.” This includes bonding and communicating with caregivers, developing self-regulation skills to cope with experiences outside the womb, and integrating and developing the sensory and motor skills needed to effectively interact, explore and play within their environment.
Part of Rehabilitation Services, the Occupational Therapy team consists of 12 inpatient occupational therapists (OTs) and six outpatient OTs who support clinics at the main campus, Chestnut Hill and Foxborough.
Pacheco, who joined the Brigham in October 2019, is the only OT for the NICU and Follow-Up Program, where she collaborates with a multidisciplinary team to promote optimal sensory and motor development in premature and medically complex babies in both inpatient and outpatient settings.
“Jessica came to us highly skilled and with excellent experience,” said Nancy Kelly, clinical supervisor for Occupational Therapy. “We’re just really thrilled that she’s been able to take on this role and perform at such a high level of skill. Because of her expertise, she was able to provide excellent care from day one.”
Pacheco was hired a few months before the COVID-19 pandemic started. While some of the hospital’s clinical services were initially scaled back at the beginning of the pandemic to limit the spread of infection, care in the NICU never stopped or slowed down. In fact, the unit saw a much higher intake of babies than ever before, and Pacheco’s work continued even when the outpatient clinic went virtual due to the pandemic.
“Being an OT in the NICU is a really unique and specialized role within the profession of OT. I feel very fortunate and grateful that my career has led me in this direction,” Pacheco said. “As an expectant mother, caregiver or parent preparing to bring life into the world, you’re not necessarily expecting or thinking your baby will begin life in an ICU setting. For families involved, it is often a traumatic, life-altering event, and we do our best as a team to help support an infant’s neurodevelopmental progression along their journey.”
Since joining the unit, Pacheco and her colleagues helped implement a standardized assessment known as the Test of Infant Motor Performance (TIMP) for infants in the NICU so that their motor skills, movements and response to visual stimulation and orientation to sound can be tracked over time, including after they are discharged. She also works to help parents and families build their confidence by teaching them how infants communicate their needs and different techniques for handling premature infants, who can be born as early as 23 weeks old.
“What’s unique about my role is my ability to work with infants and families in the NICU, and then support them in our NICU Follow-Up Program at Brigham, which allows for continuity of developmental care and skill progression,” Pacheco said.
Pacheco’s enthusiasm, collaboration and level of specialization have already made a tremendous difference for NICU patients and families, Kelly said.
“She’s just a delight to work with and I’m just so pleased that we have somebody with her expertise working with our littlest patients,” Kelly said.
Supporting Premature Infants, Families in the NICU
Pacheco always knew she wanted to have a career in the health science field. She explored different therapies and ultimately gravitated towards the field of OT, allowing her to work with individuals to support their ability to participate in daily and meaningful occupations. During her studies, she became intrigued by the work that could be facilitated in pediatrics.
“The NICU is just one setting within the many different pediatric settings you can possibly work in as an OT,” Pacheco said. “During my time as an inpatient pediatric OT, I began developing a passion for this specific population.”
Carmina Erdei, MD, a neonatologist in the Department of Pediatric Newborn Medicine and director of the Growth and Development subunit of the NICU, works with Pacheco in the inpatient setting and the NICU Follow-Up outpatient program. Erdei described Pacheco as an outstanding colleague who brings so much to the NICU environment and the outpatient program with her very valuable skill set.
“When babies are born prematurely or at neurodevelopmental risk, they often need to spend weeks or even months in the NICU. While in the NICU environment, many of these infants’ experiences and the way they’re learning about the world around them are very different from what they would be exposed to if they were healthy and at home with their families,” Erdei said. “Thanks to the work of highly skilled professionals such as Jessica, our tiny patients get the opportunity to have motor and other sensory experiences that are framed more positively. This is very important to their overall progress and recovery, and prepares infants and families for a more successful transition to home.”
Historically, Erdei said, NICUs in general have focused heavily on the medical aspects of care of fragile infants. More recently, the Brigham NICU team’s knowledge and practice have evolved to ensure these vulnerable patients also receive high-quality, expert neurodevelopmental care, including occupational therapy, to set up families for long-term success.
“We are very fortunate to have Jessica as a highly experienced and valued member of our team,” Erdei added.
Pacheco said it’s been gratifying to play such an important role in the lives of her patients and their loved ones.
“The infants and families can really integrate all of the knowledge they’ve learned in the NICU environment, take it home with them to carry on with their infant’s developmental progression, and then come to the Follow-Up clinic for additional guidance,” she said. “We meet the infants and caregivers where they’re at, and then take next steps to create goals to set them up for success once they leave the walls of the NICU and step foot into the community.”
Occupational Therapy Month is held every April to honor occupational therapists’ (OTs) substantial role in improving health and quality of life. In celebration of Brigham OTs, Brigham Bulletin is highlighting one of the many exceptional OTs to cap off Occupational Therapy Month this year.


























 “As tight-knit as we were on the General Medicine units, the COVID teams have made us even closer,” said Kelly-Makol, who has been part of the PACE Service for eight years. “When we were starting to provide care on the Special Pathogens Unit, there was a lot of anxiety. We started this group text that became a stream-of-consciousness thread for our thoughts, concerns and occasionally humor. It kept us all smiling and feeling like we weren’t alone.”
“As tight-knit as we were on the General Medicine units, the COVID teams have made us even closer,” said Kelly-Makol, who has been part of the PACE Service for eight years. “When we were starting to provide care on the Special Pathogens Unit, there was a lot of anxiety. We started this group text that became a stream-of-consciousness thread for our thoughts, concerns and occasionally humor. It kept us all smiling and feeling like we weren’t alone.”
 Since the arrival of COVID-19, the PACE Service has played a vital role in pandemic response. But when the spring 2020 surge set in, the teams quickly realized they needed more help. To manage the sharp increase in patient volume and complexity during the initial surge, about 40 PAs from other areas of the hospital were temporarily reassigned to the PA Special Pathogen Teams.
Since the arrival of COVID-19, the PACE Service has played a vital role in pandemic response. But when the spring 2020 surge set in, the teams quickly realized they needed more help. To manage the sharp increase in patient volume and complexity during the initial surge, about 40 PAs from other areas of the hospital were temporarily reassigned to the PA Special Pathogen Teams.












 Amid the immense suffering and loss during the pandemic, we have witnessed beautiful examples of compassion and human connection in every setting. I was especially moved by how nurses at the bedside comforted dying patients who were otherwise alone, without loved ones present during their final moments.
Amid the immense suffering and loss during the pandemic, we have witnessed beautiful examples of compassion and human connection in every setting. I was especially moved by how nurses at the bedside comforted dying patients who were otherwise alone, without loved ones present during their final moments.

 Tengo 18 años trabajando para tan importante hospital como es el Mass General Brigham. He pasado por momentos difíciles, como las tormentas de nieve, donde a veces no podías llegar a la casa. Pero el más difícil es esta pandemia que nos ha tocado vivir, y a pesar de todo, seguimos fuertes y con una sonrisa de esperanza. Juntos somos fuertes. Feliz navidad. We are strong.
Tengo 18 años trabajando para tan importante hospital como es el Mass General Brigham. He pasado por momentos difíciles, como las tormentas de nieve, donde a veces no podías llegar a la casa. Pero el más difícil es esta pandemia que nos ha tocado vivir, y a pesar de todo, seguimos fuertes y con una sonrisa de esperanza. Juntos somos fuertes. Feliz navidad. We are strong.

 The Operating Room (OR) facilitators are a team in the Operating Room who organize and maintain the OR desk. When the pandemic hit us hard in the spring, every one of them showed up to work every day, ready to help the team. With no questions asked, they were there to help others carry the load of the stressors everyone was facing. They are an integral part of the Operating Room who give 100 percent every day. The pride they take in their work is inspiring. They work together to strengthen the culture. I am continually impressed with their work ethic and results they produce.
The Operating Room (OR) facilitators are a team in the Operating Room who organize and maintain the OR desk. When the pandemic hit us hard in the spring, every one of them showed up to work every day, ready to help the team. With no questions asked, they were there to help others carry the load of the stressors everyone was facing. They are an integral part of the Operating Room who give 100 percent every day. The pride they take in their work is inspiring. They work together to strengthen the culture. I am continually impressed with their work ethic and results they produce.

 Shalaine Parker is a member of the Police and Security team who often plays the piano in the 45 Francis St. lobby while on break from her duties. I was there on a recent morning getting a coffee at Starbucks. It was a cold, gray November day, and when Shalaine sat down at the piano, I was startled by her incredible talent! Her music was beautiful and very soothing. I thanked her for brightening this dark day. I hope Shalaine is recognized for being a bright star at the Brigham!
Shalaine Parker is a member of the Police and Security team who often plays the piano in the 45 Francis St. lobby while on break from her duties. I was there on a recent morning getting a coffee at Starbucks. It was a cold, gray November day, and when Shalaine sat down at the piano, I was startled by her incredible talent! Her music was beautiful and very soothing. I thanked her for brightening this dark day. I hope Shalaine is recognized for being a bright star at the Brigham!
 Throughout the almost two and a half months I spent as a nurse on Shapiro 9 West, our first COVID-19 ICU, I met an angel named Lisa Beal. Lisa was an ICU extender and a fellow empathetic soul who helped create one shining moment for our patient.
Throughout the almost two and a half months I spent as a nurse on Shapiro 9 West, our first COVID-19 ICU, I met an angel named Lisa Beal. Lisa was an ICU extender and a fellow empathetic soul who helped create one shining moment for our patient.