Brigham Physicians Aid Humanitarian Response after Turkey-Syria Earthquake

Brigham emergency physician Morgan Broccoli captures this scene in İskenderun, Turkey, where she deployed with Team Rubicon to assist with disaster response after a devastating 7.8-magnitude earthquake struck the region.
On the morning of Feb. 6, Brigham emergency medicine physician Morgan Broccoli, MD, MSc, woke to the news that a 7.8-magnitude earthquake had hit Turkey and northwestern Syria. By noon, she was exchanging texts with other members of Team Rubicon, the humanitarian organization she has been involved with since 2021. A team was mobilizing, and they wanted to know if she could join.
Broccoli immediately replied: Yes. She had experience volunteering in Haiti after the 2021 earthquake and in Poland last year during Russia’s invasion of Ukraine. She also happened to be off for two days and had supportive colleagues in the Brigham’s Emergency Department who helped cover her six upcoming shifts. “Everyone in my department was amazing,” she said. “I was on a plane by 6 p.m. that same night.”
Remote Support Activated
As Broccoli headed to Turkey, several of her Brigham colleagues heeded the call to help in other ways.
“Coordination of humanitarian response efforts is complex,” explained Sean Kivlehan, MD, MPH, emergency medicine physician and director of the Emergency Health Systems Program at the Harvard Humanitarian Initiative (HHI). “On-the-ground personnel are needed to offer immediate aid, forge relationships and provide direct situational awareness while collecting key data. Remote support is important because it connects the various on-the-ground actors to ensure coordination and planning, and allows for the rapid aggregation and dissemination of data.”
As HHI’s representative to the World Health Organization’s (WHO) Global Health Cluster based in Geneva, Kivlehan works to strengthen all aspects of humanitarian response, particularly within the health sector. After the Turkey-Syria earthquake, the Health Cluster focused on sharing and analyzing data, as well as connecting health experts and partners in their networks to address urgent needs.
One of those experts was Brigham endocrinologist M. Furkan Burak, MD, who had both personal and professional ties to the country. In addition to being a native of Turkey, he served as ambassador to the U.S. for Turkey’s Ministry of Health (MoH). When the earthquake hit, Burak was devastated. “First, this is a humanitarian crisis. And second, I’m Turkish, so there I was, thousands of miles away from my country and my people. I felt helpless.”

“There I was, thousands of miles away from my country and my people. I felt helpless,” said endocrinologist M. Furkan Burak, recalling his initial reaction to the crisis in Turkey.
Advised by his friends and colleagues in Turkey not to come, Burak made the difficult decision to stay in Boston, where he leveraged his connections to serve as a local coordinator between Turkey’s MoH and the Turkish Consulate General in Boston. Providing support remotely, Burak connected with HHI and other contacts to distribute Turkey’s list of urgent health needs and ensure the right supplies were delivered to the right place as efficiently as possible.
Assessing the Needs
Broccoli and colleagues were some of the first to arrive in Turkey, where they found the country’s government requesting type 2 and 3 emergency medical teams (EMTs), which have surgical capacity as classified by the WHO, as part of their focus on the search-and-rescue effort. Team Rubicon is considered a type 1-mobile EMT, approved only to provide outpatient emergency and primary care.
“I found it remarkable that the entire world seemed to be in Turkey, wanting to help,” she said. “There were urban search-and-rescue teams from all over the world. There were also many non-governmental organizations waiting just outside the affected area to assist with medical, logistics and water, as well as sanitation and hygiene needs.”
Broccoli spent two weeks in the southern Turkish city of Adana, about 140 miles from the quake’s epicenter, where she provided the WHO with critical medical needs assessments. She attempted to travel to Syria to assist efforts there, but it was ultimately determined too unsafe. “I would have liked to do more, but the system was created for a reason,” she said.
That perspective resonated with Erica Nelson, MD, MPhil, MS, Brigham emergency medicine nocturnist and Team Rubicon’s deputy medical director, who supported Broccoli from the U.S.
“This is largely about rejecting a colonialist model of humanitarian aid,” she said. “We are not going to come in and tell you what you need, and we are not going to traverse your space without an invitation. The most effective response is when you support local infrastructure and local expertise.”
The day the earthquake struck, Nelson was putting in 60-hour weeks of clinical work in Navajo Nation through a partnership with the Indian Health Service. Even so, she managed to make time for all the backend work that is critical to any disaster response — advising on a variety of needs, including ethics, security, logistics and mobilization, and monitoring and evaluation.
Reflections in the Aftermath of Disaster
Now back at the Brigham, Broccoli, Nelson, Burak and Kivlehan have been reflecting on their recent experiences.
“Humanitarian crises, even with all of their tragedy, are remarkable for the good they bring out in society and are a reminder that while there is much work to be done, the desire to improve humanity is there,” Kivlehan said. “All of us humans are in this world together, and we need to work collectively to reduce suffering wherever it is found.”
Broccoli is currently involved in a large-scale trauma education project in Ukraine, and will continue seeking humanitarian response opportunities outside of the U.S. “While I enjoy helping offload the system in acute response, the more important work is to prepare countries to respond internally to their own disasters,” she said.
For Nelson’s part, she is now helping support a response to Cyclone Freddy in Malawi, working to support local health and WASH (water, sanitation and hygiene) infrastructure in Guatemala, and continuing to foster opportunities to build local capacity for disaster response.
Burak has a trip to Turkey planned in May, where he will visit the earthquake site and assess the mental and physical health needs of the area’s young people. He is also hoping the trip will help him further process his feelings. Since February, Burak has had flashbacks of carrying bodies after the 1999 İzmit earthquake, one of the country’s deadliest natural disasters.
“Witnessing that horrible scene as a child was what made me decide to be a doctor, because I didn’t want to feel helpless,” he said. “I know there are many things we will have to do in the days, weeks, months, years and decades ahead. We will be helpful.”





























 In recognition of the exemplary patient- and family-centered care that our Department of Obstetrics and Gynecology delivers, U.S. News & World Report named the Brigham the nation’s #1 hospital for Obstetrics and Gynecology. This recognition accompanied the news that the Brigham once again earned a spot on U.S. News’ Best Hospitals Honor Roll for 2022–23.
In recognition of the exemplary patient- and family-centered care that our Department of Obstetrics and Gynecology delivers, U.S. News & World Report named the Brigham the nation’s #1 hospital for Obstetrics and Gynecology. This recognition accompanied the news that the Brigham once again earned a spot on U.S. News’ Best Hospitals Honor Roll for 2022–23.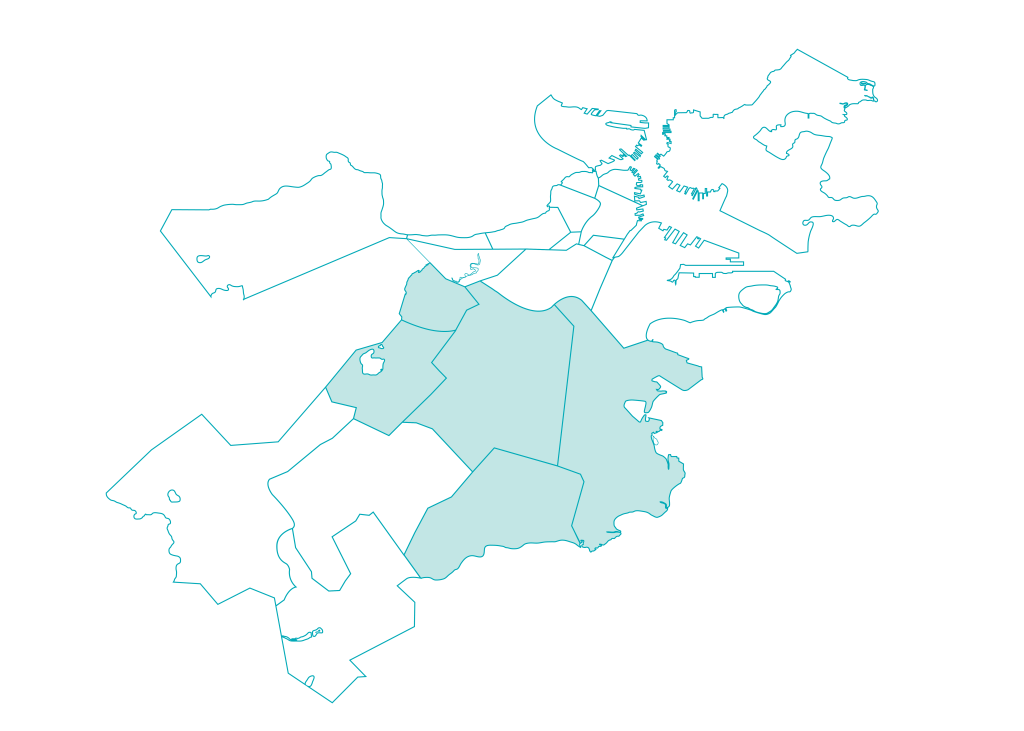 As part of our 2022 Community Health Assets and Needs Assessment, the Brigham participated in a citywide collaborative to jointly identify and address the most pressing health issues facing Boston residents. Guided by input from residents and local organizations in the Brigham’s five priority neighborhoods — Dorchester, Jamaica Plain, Mattapan, Mission Hill and Roxbury — we are partnering with community stakeholders to eliminate health inequities.
As part of our 2022 Community Health Assets and Needs Assessment, the Brigham participated in a citywide collaborative to jointly identify and address the most pressing health issues facing Boston residents. Guided by input from residents and local organizations in the Brigham’s five priority neighborhoods — Dorchester, Jamaica Plain, Mattapan, Mission Hill and Roxbury — we are partnering with community stakeholders to eliminate health inequities.

 Last summer, physician-scientists from the Brigham presented new evidence that drugs originally developed to treat type 2 diabetes may benefit a wide range of patients experiencing heart failure. Brigham investigators helped lead the largest clinical trial to date on a broad range of patients with heart failure, finding that a class of drugs known as SGLT2 inhibitors provided protection from cardiovascular events.
Last summer, physician-scientists from the Brigham presented new evidence that drugs originally developed to treat type 2 diabetes may benefit a wide range of patients experiencing heart failure. Brigham investigators helped lead the largest clinical trial to date on a broad range of patients with heart failure, finding that a class of drugs known as SGLT2 inhibitors provided protection from cardiovascular events.

 I am extraordinarily proud of all that we accomplished in 2022 to deliver expert and compassionate care, drive research and innovation, train tomorrow’s health care professionals and care for our communities.
I am extraordinarily proud of all that we accomplished in 2022 to deliver expert and compassionate care, drive research and innovation, train tomorrow’s health care professionals and care for our communities.







 Over the past year, I have quickly become aware of how special our health care providers — including nurses, doctors and other care team members — are in taking care of our patients and their families. And now through personal experiences for me and my family, I further recognize the high-quality and compassionate care our organization provides. Recognizing what all of our patients and their families already know, our Brigham family delivers world-class care with outstanding compassion and dedication to our community and its well-being. Thank you for all that you do.
Over the past year, I have quickly become aware of how special our health care providers — including nurses, doctors and other care team members — are in taking care of our patients and their families. And now through personal experiences for me and my family, I further recognize the high-quality and compassionate care our organization provides. Recognizing what all of our patients and their families already know, our Brigham family delivers world-class care with outstanding compassion and dedication to our community and its well-being. Thank you for all that you do.



 I will always remember the feelings of joy and anticipation I felt upon learning that a new president had joined our BWH family. At the first town hall meeting, we had the opportunity to meet Dr. Higgins and ask him questions. I welcomed him, of course, and then told him, “Roll up your sleeves and let’s get to work.” His response felt genuine and comforting because I saw in him a leader of color, which makes me so very proud, and someone who is exceedingly qualified to lead this great institution!
I will always remember the feelings of joy and anticipation I felt upon learning that a new president had joined our BWH family. At the first town hall meeting, we had the opportunity to meet Dr. Higgins and ask him questions. I welcomed him, of course, and then told him, “Roll up your sleeves and let’s get to work.” His response felt genuine and comforting because I saw in him a leader of color, which makes me so very proud, and someone who is exceedingly qualified to lead this great institution!
 A few weeks ago, I was covering our Radiation Oncology urgent patient service in our Boston clinic, and the number of simulation, or “sim,” appointments crept up to nearly 100 for the week. These are the radiation mapping appointments that precede every patient’s course of radiation treatment. Just a few years ago, seeing 100 sims in a week would have been unthinkable and unmanageable for us.
A few weeks ago, I was covering our Radiation Oncology urgent patient service in our Boston clinic, and the number of simulation, or “sim,” appointments crept up to nearly 100 for the week. These are the radiation mapping appointments that precede every patient’s course of radiation treatment. Just a few years ago, seeing 100 sims in a week would have been unthinkable and unmanageable for us.







 There are many moments that I look back on this year, but my favorite was my very first day at Brigham and Women’s Hospital. I began my journey here this past January as a radiology tech aide — my very first job in a hospital. To say I had little experience under my belt would be an understatement. But soon enough, and with the help with my fellow CT techs, I caught on. My co-workers not only modeled how to do the job, but they also, most importantly, demonstrated empathy and compassion. I knew then that I was exactly where I was meant to be — here at BWH.
There are many moments that I look back on this year, but my favorite was my very first day at Brigham and Women’s Hospital. I began my journey here this past January as a radiology tech aide — my very first job in a hospital. To say I had little experience under my belt would be an understatement. But soon enough, and with the help with my fellow CT techs, I caught on. My co-workers not only modeled how to do the job, but they also, most importantly, demonstrated empathy and compassion. I knew then that I was exactly where I was meant to be — here at BWH.
 One of the highlights from this past year was organizing a series of events with Diana Reusch, MD, a pediatric dermatology fellow at Boston Children’s Hospital, to expose 45 middle and high school students to medicine. These students were able to concentrate on perfecting their running stitch, identifying organs using an ultrasound, honing their laparoscopic surgical skills and learning the importance of personal protective equipment. This collaboration was with a summer youth program of the Phillips Brooks House Association (PBHA), a student-led community service organization at Harvard University with yearlong programming for local underserved youth in the Boston and Cambridge area. Over the summer, there are 11 neighborhood-based camps that offer quality programming and professional development to provide valuable work experiences and positive social connections in a safe, inclusive environment. We were able to work with teenage students involved in PBHA’s Junior Leaders in Communities (JLinc) and LEADERS Program. It was exciting to meet them, show them around the Longwood Medical Area and teach them about careers in medicine.
One of the highlights from this past year was organizing a series of events with Diana Reusch, MD, a pediatric dermatology fellow at Boston Children’s Hospital, to expose 45 middle and high school students to medicine. These students were able to concentrate on perfecting their running stitch, identifying organs using an ultrasound, honing their laparoscopic surgical skills and learning the importance of personal protective equipment. This collaboration was with a summer youth program of the Phillips Brooks House Association (PBHA), a student-led community service organization at Harvard University with yearlong programming for local underserved youth in the Boston and Cambridge area. Over the summer, there are 11 neighborhood-based camps that offer quality programming and professional development to provide valuable work experiences and positive social connections in a safe, inclusive environment. We were able to work with teenage students involved in PBHA’s Junior Leaders in Communities (JLinc) and LEADERS Program. It was exciting to meet them, show them around the Longwood Medical Area and teach them about careers in medicine.










