From the OR to the Swiss Alps, mom of 4 with rare brain disorder on path to healing thanks to Brigham and Spaulding care teams

Jennifer Murff and her husband, Justin, before her first neurosurgery at the Brigham in August 2022.
After speaking at a conference in Sweden in May 2022, Jennifer Murff, PhD, MA, was stepping off the stage when she was struck by what felt like the worst headache of her life.
It must be the adrenaline, she thought to herself.
But the tremendous pressure, like a vice around her skull, refused to stop. Even after her long flight home to Virginia, she was still in agony. Her mother-in-law pleaded with her to go to the emergency room.
Murff tried to brush her off. “I figured it was a migraine. You don’t need to go to the hospital for a migraine,” she said.
Eventually, she relented. That was when Murff heard two words — arteriovenous malformation — that would upend her life as a busy mom of four and president and CEO of an international Christian ministries organization.
Also known by its acronym, AVM, the condition causes capillaries — tiny blood vessels that connect veins and arteries — in the brain to form incorrectly. In a healthy person, brain capillaries are like speed bumps on a busy road, preventing blood from flowing too quickly across these connections. In someone with an AVM, blood rushes from the artery into the vein, causing it to expand like a balloon.
At any time, the pressure buildup from an AVM can cause the vein to burst without warning. If that happens, there is a 20 percent chance of death. Among those who survive, the risk of permanent injury to the brain is greater than 40 percent.
AVMs are rare, affecting one in 100,000 people, and congenital, meaning they are present from birth. They are the leading cause of hemorrhagic stroke in young people.
For Murff, the news got more discouraging from there. AVMs are categorized from grade 1 to grade 5 according to their size and complexity, with grade 5 being the most difficult and dangerous to remove. Hers was a grade 5 — large and located deep in her brain, perilously close to the neurons that control sensory-motor functions, vision and language. She saw several prominent neurosurgeons around the country. All declined to operate. It was just too risky, they told her.
“I thought, I’m a mom. I have four daughters. I have something to live for. I have a wonderful husband. I have a great career and feel like I’m on a mission,” she said. “I have so much to offer and so much more to do. I can’t die.”
‘Her spirit seemed unbreakable’
In the ensuing weeks, during one of her many journeys into the depths of Google search results, Murff came across a Brigham Bulletin article that bore striking similarities to her own story. It was about another mother of four with an AVM, Nicole Haight, who had been told repeatedly that her case was inoperable — but this story had a different ending. Haight was eventually treated and cured, thanks to the expert care she received at Brigham and Women’s Hospital.
Murff wasted no time connecting with Haight on social media to learn more about her experience. Encouraged by their conversation, she contacted Haight’s neurosurgeon, Nirav Patel, MD, director of the Brigham’s AVM program and a global expert in treating the most complex AVMs. Their first Zoom meeting a few days later would mark the start of a long but hopeful new chapter — one filled with triumphs, setbacks and, ultimately, healing.
“What I love about Dr. Patel is he was very honest. He didn’t sugarcoat anything. Although you can’t always foresee complications, I knew what I was getting into and that Dr. Patel was the right surgeon for me,” Murff said. “I had such peace that I was going to be OK at the end of this.”

Murff and her husband share a moment with members of their care team on Braunwald Tower 9CD.
In all, Murff underwent 10 surgeries with Patel and his team. She had to relearn how to talk and walk, milestones she achieved with the support of her interprofessional care team at Spaulding Rehabilitation, where she completed inpatient rehabilitation after her first three surgeries in August 2022.
Today, Murff is free of her AVM. Her mind and body have largely recovered, with few visible traces of the trauma both underwent over the past two years.
“The hardest thing was realizing that I was going to have to regain some cognitive functions. My brain is the fabric of my personality, my career — everything,” Murff said. “I remember after surgery wanting to call my husband, but I couldn’t figure how to put my password into my phone. I started weeping. ‘Is this what I signed up for? I signed up to be healed.’ I decided right then to pull myself together, and my faith played a huge role in that because I believe God was in the operating room with Dr. Patel.”
Last July, just three and a half months after her last surgery, she traveled to California to present an academic paper on a topic that bore new meaning in her life: resiliency. There, she met a couple from Switzerland who invited Murff and her family to hike the Swiss Alps with them. In November, they did just that. At one point during their hike, Murff turned around to see that her husband was crying. They were tears of joy upon witnessing how far she’d come.

Eight months after her last surgery, Murff hikes the Swiss Alps.
Her strength, courage and extraordinary recovery have left a lasting impression on her care team, too.
“Whenever I see an AVM, the first question I ask myself is, can I do this? Am I physically capable? If the answer is yes, the second question I ask myself is, should I do this? And the ‘should’ is wrapped up in the other person — the patient,” Patel said. “I told Jennifer this was going to be a very difficult operation with a high risk for lasting complications. Her spirit was emboldened by concern a mother has for her children and her faith in God. After understanding the risks on both sides, she made the best decision for her situation and went forward confidently.”
Spaulding physical therapist Rebecca Phelan, DPT, was also moved by her experience caring for Murff and helping restore her mobility.
“Even now, almost two years later, I can still remember the feeling of walking into Jenn’s room for her treatment sessions because of how good the energy always was. She exuded such positivity and remained so motivated for our therapy sessions, even when I knew she was exhausted,” Phelan said. “You always wish for the best outcomes for your patients, but there’s nothing like experiencing their successes alongside them in the journey of their recovery.”
Precision and determination
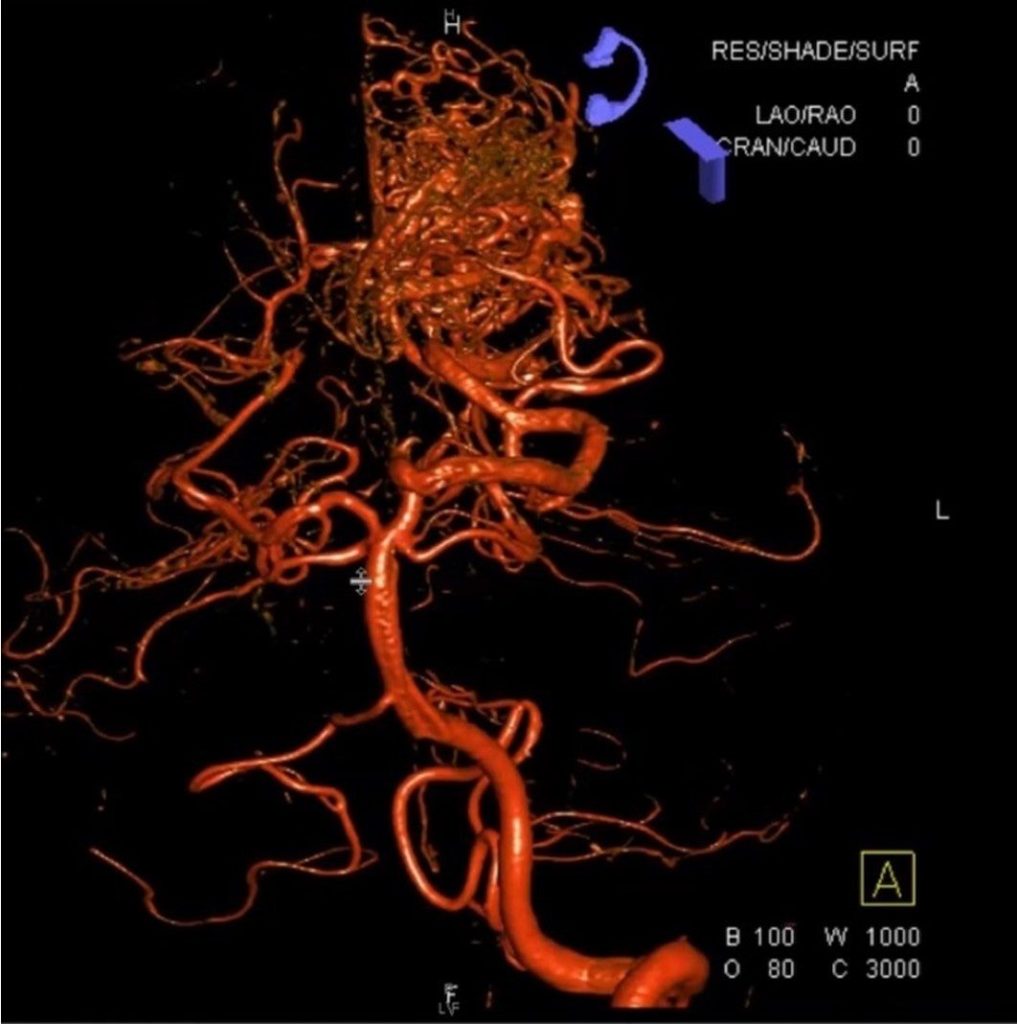
Imaging illustrates the AVM’s intertwined blood vessels prior to Murff’s first surgery.
Surgical removal of an AVM is a slow, delicate process. The entire surgery is performed under a microscope as a multidisciplinary team works to untangle and remove the malformed blood vessels, millimeter by millimeter.
In the Operating Room, the surgical team first closes arteries that feed the AVM and then begins to remove it. To confirm the removal is complete, the team performs an angiogram in the Interventional Suite.
For Murff’s procedure, the highly specialized, multidisciplinary team included neurophysiologist Mitali Bose, MS, CNIM, who continuously monitored Murff’s brain activity during the surgery to maximize safety and preserve function.
“Neuromonitoring doesn’t take away all risk, but it gives the surgeon a lot more confidence,” Patel explained. “For example, Mitali would let me know when I was 3 millimeters away from her motor fibers.”
For moderately sized AVMs, the removal process can take up to 12 hours. For Murff, it took double that time — performed as three separate surgeries over seven days. What made a complete removal especially difficult, beyond it being a high-grade AVM, was that her AVM was diffuse, Patel explained. In other words, instead of being a single, compact mass, it was spread out in the brain with long tendrils.
“Each time I’d finish, I’d think, ‘OK, I got it,’ and then I’d go into the angio suite and see there was still some left,” Patel said.
Sharing a victory lap
Given the enormous physical toll of the multiple brain surgeries, Murff remained sedated in the Neurosciences Intensive Care Unit (ICU) with one-to-one nursing care between operations. Neuro ICU nurses vigilantly monitored her blood pressure and adjusted IV drips around the clock to keep it at a safe level.
After her third surgery, the team breathed a sigh of relief. The AVM was finally gone. Now, Murff would face a difficult road to recovery, one that included complications from surgery, additional procedures to treat them and inpatient rehabilitation. In all, she and her family spent more than three months in Boston, followed by more inpatient rehabilitation back in Virginia.
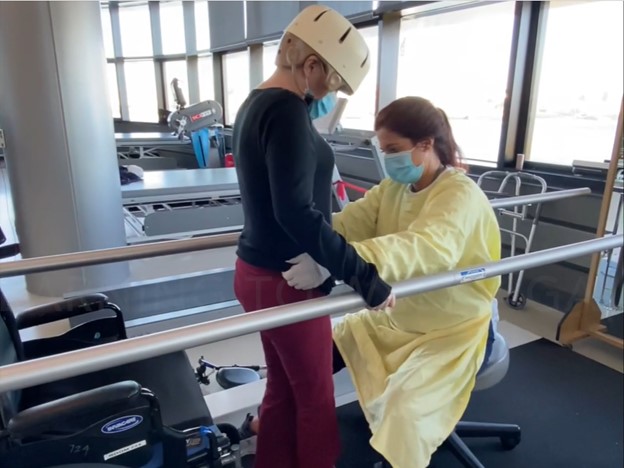
Murff participates in a physical therapy session with Rebecca Phelan at Spaulding.
No matter the setback, Murff was determined to get better. Reflecting on the day she was discharged from the Brigham to Spaulding, Murff recalled taking “a victory walk” with Patel around the ICU.
“I didn’t know any of the nurses because I was very sick when I was with them. But when they saw me, they would just cry. They said, ‘You were our hardest case, and now you’re walking and flourishing,’” Murff recalled. “I thought that victory walk was just for me, but it was for everyone.”
As a physical therapist, Phelan explained that helping patients achieve their mobility goals is about more than moving the body. It’s also helping them find their own strength within.
“When I see individuals for therapy, they’re often experiencing one of the most trying times of their lives,” she said. “In my experience, patients can have a hard time seeing the progress they are making because they are constantly comparing their current level of function to the level they were at prior to their medical event or condition. It’s always been important to me to encourage my patients by highlighting even the smallest amount of progress because of the resultant confidence it gives them to continue working hard in therapy and courage to navigate their new normal.”
Now, almost two years out from the circumstances that brought her to the Brigham and Spaulding, Murff said she will never forget the exceptional and compassionate care she and her family received.
“The people at these hospitals weren’t just providing a service to me. I love them, and I hope they felt seen just like they made me feel seen and cared for,” she said. “When you’re dealing with issues of the brain, you just need your dignity. And I felt like I maintained my dignity at every stage, whether I was at Brigham or Spaulding. That was really special.”

6 Responses to “From the OR to the Swiss Alps, mom of 4 with rare brain disorder on path to healing thanks to Brigham and Spaulding care teams”
I love you, Jenn. I am so thankful you didn’t give up and continued forging on. My determined Young Lady 🙂
Dear Jennifer,
I was so inspired by your story. In 2001, I was diagnosed with severe Chiari malformation and over the last 20+ years I’ve undergone many brain surgeries as well; had to learn to walk and write again. Ironically I was a neuro physical therapist before all this began. I also have Ehlers-Danlos syndrome which has resulted in multiple disc, spinal cord and shoulder surgeries. I’m currently fused from my skull-T1. My breast cancer story is another God story as well!
My three sons were 7 and my twins were 5 went I went through my first brain surgery and they were 26 and 24 when I went through my last in 2020. Like you, I’m also blessed with an amazingly supportive husband who has held my hand through all of this. Although I’ve regained much of my physical function I still deal with daily headaches-sometimes severe/debilitating.
I too am a Christ follower and I don’t know what I would do without Him as my foundation, anchor, Rock, and Savior. He is the reason for my hope and gives me the strength to press on each day, to pray for others, and to share (like you) that pain has purpose.
I don’t know if you have heard of Katherine and Jay Wolf, but many years ago Katherine experienced a stroke due to an AVM months after giving birth. If you haven’t heard/read their story, go to hopeheals.com.
Praising the Lord for your healing!
In His Gracious Grip,
Amy
Dear Amy,
I am so moved by hearing your story. I’m so thankful for your strength and endurance as well as your faith in God.
I have read Katherine’s book. It was powerful. She encouraged my heart as I was going through this journey. I am thankful that we are not alone.
I hope that I can meet you one day.
You’re a rockstar, Jenn!
Amazing! I feel so fortunate to have read this today! Continued blessings!!
God’s grace and mercy are evident in Jennifer Murff’s remarkable journey from the OR to the Swiss Alps! Her strength and perseverance are a testament to the power of faith and resilience. We praise God for the skilled and compassionate care teams at Brigham and Spaulding who played a vital role in her healing. And a special thank you to her husband, who has been a rock for her throughout this journey – his love and support have undoubtedly been a source of comfort and strength. May Jennifer’s story inspire hope and encouragement to all who face challenges!
God bless,
Sama
Comments are closed.