Brigham NICU’s Small Baby Program, the First of Its Kind in Massachusetts, Helps Tiny Preterm Infants Thrive
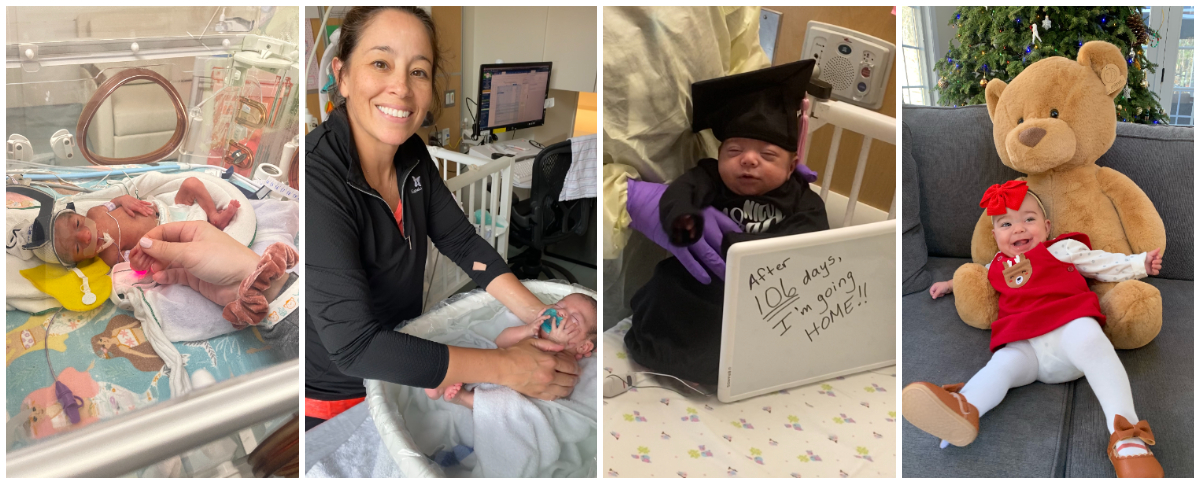
Baby Olivia, who weighed less than 2 pounds at birth, was among the first infants enrolled in the Brigham NICU’s Small Baby Program, which delivers highly specialized care to tiny preterm infants. Now 8 months old, she is thriving.
When Victoria’s water broke 23 weeks into her pregnancy, she knew that her daughter Olivia would likely arrive prematurely. Despite the frightening circumstances, Victoria, who was already planning to deliver at the Brigham, was reassured to know that she and her baby would be in the best hands in the hospital’s Neonatal Intensive Care Unit (NICU).
Olivia was born in April 2023 at 26 weeks and weighed 1 pound and 11 ounces, which classified her as a “tiny preterm infant.” Her birth happened to coincide with the launch of the NICU’s Small Baby Program, which specializes in caring for tiny preterm infants like Olivia. It is the first program of its kind in Massachusetts.
The program, which is dedicated to the care of infants born at 22 weeks’ gestation and up, or those weighing less than 1,000 grams (about 2.2 pounds), first took root in 2022. It brings together a team of multidisciplinary professionals including dieticians, respiratory therapists and pharmacists whose unique expertise provides very premature babies with the specialized care and monitoring they need to thrive.
In collaboration with the Department of Obstetrics and Gynecology, the Brigham NICU cares for more extremely-low-birthweight babies born in Massachusetts than any other hospital in the state.
For Victoria, a mother of three but first-time NICU parent, the special expertise and family-centered approach of the Small Baby team made the uncertainties of Olivia’s stay far more manageable.
“I thought it was awesome. She had a nutritionist, physical therapist and respiratory therapist,” said Victoria, who requested that only her first name be used. “There was always somebody we could speak with who specialized in a specific area and could really break it down in layman’s terms for us.”

Baby Olivia snoozes in the arms of NICU nurse Kerri Duggan.
Elizabeth Flanigan, MD, MBA, MPH, chief of Clinical Operations in the Department of Pediatrics, said the NICU team saw an opportunity to elevate the care they already provided to very premature infants with a more standardized approach.
“We were actually already taking care of these babies. We just weren’t doing it in a focused way that treated these particularly small babies as a unique population who needs special attention paid to those differences,” Flanigan said. “The goal of the program is not only to have these babies survive, but also achieve the best possible outcomes and thrive within their families and communities.”
Personalized Care
One hallmark of the program is each baby receives a designated, primary neonatologist who is assigned 24 to 72 hours after birth and follows them for the entirety of their stay in the NICU — providing continuity for both the family and medical team.
“There are so many emotional ups and downs within the NICU course that a primary neonatologist really bridges not just the medical care but also that emotional, psychological care for the families,” said Elisa Abdulhayoglu, MD, MS, medical director of the NICU. “As the primary neonatologist, sometimes all you do is sit there and listen to the families express their concerns, frustrations, fears and hopes.”
While Olivia was in the NICU, Victoria visited her every day, a practice that also enabled her to build a close relationship with the care team.
“I owe everything to them. They took care of my daughter like she was their own,” Victoria said. “I was there every single day, all the time, and there was definitely a big, big level of trust there.”
Each interprofessional team caring for a tiny preterm infant in the program consists of a variety of specialists across multiple disciplines dedicated to delivering individualized care for both the baby and family. In addition to physicians and nurses, the team also includes respiratory therapists, nutritionists, physical therapists, occupational therapists, speech therapists, social workers, neonatal pharmacists and parent support specialists — all of whom come together to make the NICU experience as smooth as possible.
“The amount that we have to take into consideration for these tiny babies is enormous,” Abdulhayoglu said. “If you see the team on morning rounds with one of these babies, particularly in the first couple of weeks when the babies are so fresh and so critical, the amount of collaboration and attention to detail are incredible — all the calculators that are out, making sure that every last CC or one hundredth of a CC is counted for and appropriate.”
‘The Sky’s the Limit’
One year since the program’s launch, the team is now starting to see improvements in the outcomes of tiny preterm infants who are a part of the Small Baby Program. Flanagan said that not only are more babies surviving, but they are thriving with a low likelihood of long-term significant impacts.

“They took care of my daughter like she was their own,” says Victoria, pictured above with her family, about Olivia’s NICU care team.
“The sky’s the limit on what these babies are going to achieve,” Flanigan said. “We have real optimism for how these babies are going to do in the future, and we see that optimism reflected in the families and the way they interact with their babies.”
After any baby is discharged from the NICU, their team continues to monitor their progress and support the family with the transition to home.
“Olivia’s had follow-up visits with various different specialists just to check in and see how she’s doing,” Victoria said. “I really appreciate that they don’t just discharge you and then that’s it.”
Olivia was discharged from the NICU after three and a half months with no need for breathing or feeding support –– just as “a little baby,” Victoria said. Now 8 months old, she’s hitting milestones for her corrected age, including rolling both ways, reaching and grabbing things with her hands, babbling, holding her head up and trying solids for the first time recently. Victoria continues to share these updates with members of Olivia’s NICU team.
Flanigan said the team’s collaborative approach and broad range of expertise are crucial to achieving outcomes like this.
“It’s kind of like if you’re going on a journey in the dark and you have a flashlight, every team member that comes in is adding another light source,” Flanigan said. “The path becomes clearer and clearer, and we’re really now getting to the point where whole path is being illuminated around this baby and this family.”

One Response to “Brigham NICU’s Small Baby Program, the First of Its Kind in Massachusetts, Helps Tiny Preterm Infants Thrive”
My almost 24-year-old daughter was born and cared for as a micro preemie (15 ounces!) at BWH and the NICU. I daresay that she received the best care there that she could have ever received. That the teams at the NICU wanted to enhance their already above the line care gives me much hope in humanity, in times when there’s so much turmoil in the world. My daughter is a thriving, healthy adult and I am so thankful to all the BWH people who were instrumental in her care for the 3.5 months we lived at the NICU!